3D Bioprinting in Advancing Cancer Treatment
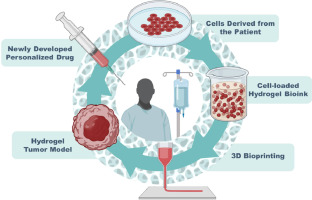
The field of cancer research is undergoing a remarkable transformation, thanks to the innovative approach of 3D bioprinting. This cutting-edge technology is paving the way for more accurate and realistic tumor models, which have the potential to revolutionize radiotherapy. Researchers are now able to create lifelike 3D replicas of tumors that mimic the tricky parts of real human tissues. Unlike traditional two-dimensional cell models that overlook many of the hidden complexities of tumor behavior, these three-dimensional representations offer a deeper understanding of the subtle parts of cell-to-cell interactions, such as how immune responses and vascular functions operate during treatment.
By stepping into this new era, scientists and clinicians aim to improve cancer treatments and enhance patient outcomes. This opinion editorial explores the developments made by researchers at a leading medical physics lab, examines the significant potential of 3D bioprinted tumor models, and discusses how these advancements are reshaping future therapies for cancer patients.
Embracing the Future: How 3D Bioprinting is Changing Cancer Research
Over the past few years, the use of 3D bioprinting methods in cancer research has grown rapidly. At the heart of this advancement is the work being done in university labs, where researchers tackle the complicated pieces of tumor biology and radiotherapy. By using bioprinters, they can recreate tumors with realistic structures including vasculature, blood flow, and perfusion. These lifelike models provide a more true-to-life environment that better captures the tiny details of how tumors respond to treatments. This innovative approach has opened doors to improving radiotherapy techniques and making cancer therapies more precise.
Traditional two-dimensional cell cultures served as the foundation for early radiation dose calculations. However, these models often oversimplify the tangled issues present within an actual tumor. They fail to consider the off-putting challenges involving immune responses and blood vessel interactions. In contrast, 3D bioprinted models can be made to include these aspects, thereby allowing researchers and physicians to test different radiotherapy and chemical therapy techniques more accurately. This shift not only highlights a technological leap but also shows a deep commitment among scientists to find more effective cancer treatments.
3D Printed Tumor Models for Accuracy in Radiotherapy
One of the exciting developments in cancer treatment innovations is the refinement of radiotherapy using 3D printed tumor models. With conventional methods, patients often receive uniform doses of radiation over a period of weeks. These methods sometimes miss out on the fine shades of interaction between charged particles and living tissue. Using realistic 3D models, researchers can simulate the effect of localized high doses—a strategy that could provoke a more robust immune response against the tumor.
This approach provides critical insights into the way tumors react when subjected to various radiation patterns. In such models, scientists can scrutinize the effects of radiation on both the tumor’s structure and its surrounding environment, offering a clearer picture of how to “figure a path” through the complexities of cancer treatment. The data derived from these experiments holds the promise to guide clinicians in choosing therapies that are super important for optimizing patient survival.
Radiotherapy Techniques: Rethinking Dose Delivery
One emerging strategy involves experimentations with non-uniform radiation doses. Instead of the traditional method of delivering small, consistent doses over time, researchers are examining whether higher doses delivered selectively can better disrupt tumor growth. This idea has generated much debate in the medical community as it challenges conventional approaches and tests the limits of both radiotherapy and bioprinting technologies.
Physicists and oncologists alike are enthusiastic about the possibility of “taking a closer look” at the cellular response to these new dose patterns. Several key factors are being considered in these studies:
- Localized Radiation Impact: Assessing whether targeted high doses result in more effective tumor regression.
- Immune System Activation: Evaluating if this method triggers a strong immune response that could prolong patient survival.
- Side Effects Minimization: Analyzing the potential of these techniques to reduce collateral damage to surrounding healthy tissues.
Such studies involve rigorous testing with the aid of 3D bioprinted models, which provide a trusty platform for getting into the effects of varied radiation techniques. By focusing on the nitty-gritty details of these outcomes, medical professionals hope to design radiotherapy protocols that are not only more efficient but can also be customized to the specific needs of individual patients.
Innovative Research Approaches in Medical Physics
Modern medical physics has evolved into an interdisciplinary field where technology meets biology in surprising and promising ways. Researchers in this area are actively working through the challenging parts of cancer treatment research. In labs led by experienced professors, teams composed of graduate students and undergraduates collaborate to improve the methods used in radiation therapy.
This kind of cross-level collaboration ensures that young researchers get hands-on experience with state-of-the-art technologies like 3D bioprinting. For many budding scientists, the exposure has been transformative, allowing them to pick up essential technical skills and enhance their communication proficiency. Mentorship in these labs plays a crucial role in paving the way for a new generation of medical physicists who are ready to face the overwhelming challenges of modern healthcare.
Training Tomorrow’s Experts Through Hands-On Experience
The journey toward mastering 3D bioprinting and advanced radiotherapy techniques has been enriched through active mentorship and research collaboration. Graduate students and undergraduates working closely together form an integral part of the lab’s ecosystem. This blend of experience and curiosity has driven innovation and inspired participants to “dive in” and explore new methods of treating cancer.
For instance, one insightful student has been examining how varying radiation levels affect the elasticity and viscosity of tumor models. His research isn’t just a laboratory exercise; rather, it provides a detailed glimpse into how the physical properties of tumors might influence their response to treatment. With each experiment, researchers aim to decode the little twists and slightly different aspects of tumor biology, which can ultimately lead to better therapeutic strategies tailored to each patient’s unique condition.
The lab’s environment reinforces the idea that learning by doing is super important. Not only do students get the opportunity to work with the latest technology, but they also witness the immediate real-world impact of their work. Such exposure prepares them for clinical roles where they will be standing on the front lines, directly contributing to the evolution of cancer care.
Breaking Down the Challenges: The Tricky Parts of Tumor Research
No scientific endeavor is without its share of tricky parts and tangled issues. In the world of cancer research, one of the most nerve-racking challenges is bridging the gap between laboratory models and the actual human body. Traditional methods have often fallen short because they miss out on important aspects of tumor behavior, such as the impact of immune cells and blood vessel dynamics.
3D bioprinting addresses these hidden complexities in several ways:
- It replicates the vascular network of human tissues, which is crucial for simulating how tumors receive nutrients and oxygen.
- It allows researchers to account for the perfusion and blood flow that plays a role in how drugs or radiation disperse through the tissue.
- It enables precise observations of cell-to-cell interaction phenomena that are otherwise too subtle to detect in simpler models.
This technology helps scientists “find your way” through the many twists and turns of tumor behavior that were once too confusing to study in detail. By converting these complex biological systems into standardized laboratory models, researchers can now experiment with confidence and greater reproducibility.
Integrating Alternative Approaches in Cancer Therapy
While radiotherapy is a cornerstone of cancer treatment, it’s not the only method under scrutiny. Alternative strategies—ranging from the use of innovative chemotherapy techniques to complementary natural therapies—are being considered in tandem with radiotherapy to design more effective treatment plans. The integration of these varied approaches is a holistic step forward in managing cancer care.
For example, 3D bioprinted models have been used in prior studies mainly to test the effects of chemotherapy drugs. Now, the same technology is being translated to improve radiotherapy techniques. This multidisciplinary approach ensures that multiple methods are evaluated concurrently, ultimately benefiting the patient by combining the best attributes of each strategy.
Some potential benefits of integrating these alternative methods include:
- Enhanced Treatment Efficacy: Combining radiotherapy with chemotherapy or natural supplements may yield better tumor response rates.
- Reduced Side Effects: A more targeted treatment plan may result in fewer adverse side effects, improving the quality of life for patients.
- Personalized Therapy: The ability to model individual tumors in 3D opens doors for highly customized treatment regimens that are tailored to the unique features of a patient’s cancer.
This holistic approach to cancer treatment encourages clinicians to “take a closer look” at the patient as a whole rather than relying solely on one standard method. It recognizes that the body is a complex system where various treatment modalities may work together to achieve the best outcomes.
Exploring Real-World Implications for Patient Care
The implications of research conducted with 3D bioprinted tumor models extend far beyond the laboratory. For patients, the promise of more effective and tailored treatments represents hope in the face of a terrifying diagnosis. As advances in radiotherapy continue to evolve, the potential for increased survival rates and improved quality of life becomes more tangible.
Patients and their families are watching with interest as these technologies move from bench to bedside. While the research is still in its developmental stages, early findings suggest that these models could eventually help clinicians:
- Customize Radiation Protocols: By predicting how a tumor will respond to certain radiation patterns, doctors can adjust the dosage and timing for maximum effectiveness.
- Reduce Collateral Damage: More precise targeting could minimize injury to adjacent healthy tissues, reducing the side effects often associated with radiotherapy.
- Boost Immune Responses: The potential to trigger robust immune responses through targeted high-dose radiation could add an important new tool in the fight against cancer.
These advances encourage a future where treatment is not only more accurate but also more humane, addressing the complex needs of diverse patients. By providing a finer lens through which to examine tumor behavior, 3D bioprinting helps bridge the forward-looking gap between experimental research and practical medical applications.
Medical Physics: A Team Effort for Breakthrough Discoveries
Modern medical physics is not a solitary pursuit; it’s a vibrant community of motivated researchers, experienced clinicians, and passionate students all working together. The collective effort in labs has led to groundbreaking advances in designing therapeutic techniques that are super important in the fight against cancer.
This collaborative environment is marked by continuous learning, where mentors play a crucial role in guiding novices through the sometimes overwhelming maze of advanced technology and biological research. In these settings, young scientists are not only learning technical skills but are also being equipped with the communication skills necessary to share their findings with a broader audience. These experiences are laying the groundwork for a future in which medical physics is increasingly patient-focused and solution-driven.
Here are a few ways in which teamwork is shaping research innovations:
- Interdisciplinary Training: Bringing together minds from physics, biology, and engineering to tackle real-world healthcare problems.
- Practical Skill-Building: Offering hands-on projects that enhance technical abilities in 3D bioprinting and data analysis.
- Mentorship Programs: Establishing supportive networks where experienced researchers guide the newcomers in adapting to emerging technologies.
Such initiatives ensure that students, whether they are undergraduates or graduate candidates, get a chance to see first-hand how theoretical knowledge can be applied to treat diseases affecting millions. These opportunities are key in “figuring a path” through the challenges of medical research and, ultimately, in developing life-saving treatment methodologies.
Overcoming the Challenges of Translating Laboratory Success to Clinical Practice
The journey from laboratory research to clinical application is often loaded with challenges. One of the major hurdles in this transition is ensuring that the promising results seen in 3D bioprinted models truly represent what will happen inside the human body. Although these models capture an impressive array of the subtle details of tumor biology, scaling these findings for patient care requires further studies and careful clinical trials.
To overcome these issues, researchers must consider several important factors:
- Standardization of Models: Developing protocols that ensure each 3D bioprinted tumor consistently replicates the key features of real tumors.
- Clinical Validation: Conducting rigorous trials to confirm that the experimental outcomes can be successfully mirrored in patient settings.
- Interdisciplinary Communication: Maintaining an open dialogue among physicists, oncologists, radiologists, and biologists to seamlessly transition innovations into clinical practice.
The translation process involves a series of stepping stones, from controlled lab experiments to expansive clinical studies. Each stage must be carefully managed to mitigate risks and ensure that the new techniques do more good than harm. This journey, while making its way through the maze of systematic obstacles, highlights the essential need for collaboration between research teams and clinicians.
Understanding the Biomechanics of Tumors Through 3D Models
Another fascinating area of research using 3D bioprinted tumor models is the examination of the physical, or biomechanical, qualities of tumors. Research reveals that properties like elasticity and viscosity—fancy terms that essentially measure how a tumor might respond to pressure or deformation—play a significant role in how a tumor reacts to radiotherapy.
By studying these biomechanical characteristics, researchers can get into the fine points of tumor regression. Understanding these aspects provides a clearer picture of how radiation affects not only the cancerous cells but also the surrounding supportive tissues. This knowledge could aid in refining dosage delivery to maximize the impact on the tumor while safeguarding adjacent healthy tissues.
Some specific biomechanical insights include:
- Elasticity: Reflects how well the tumor adapts to physical changes, potentially influencing how radiation-induced shrinkage occurs.
- Viscosity: Provides clues about the tumor’s internal resistance to deformation, which might affect how energy is absorbed during treatment.
- Structural Integrity: Offers a snapshot of how the tumor maintains its shape and function, which is critical when assessing the overall treatment efficacy.
Examining these properties enables researchers to “make your way through” the tricky parts of tumor behavior, ultimately leading to more targeted radiotherapy plans. As these studies progress, the insights gained will likely influence the development of new therapeutic protocols that take into account not only chemical and radiation factors but also the physical characteristics of the tumors.
Integrating Data and Technology: The Role of Bioprinting in Personalized Medicine
Personalized medicine has become a buzz phrase in healthcare circles as clinicians strive to meet each patient’s unique needs. With the advent of 3D bioprinted tumor models, personalized radiotherapy is quickly evolving from an ambitious goal into an achievable reality. By integrating detailed data from these models, doctors can tailor treatment plans that account for the minute details of tumor structure and behavior.
This approach harnesses the power of technology to “sort out” the many moving parts involved in delivering effective cancer therapy. As each tumor has its distinct profile, doctors can use information gleaned from bioprinted models to:
- Customize radiation dose patterns based on the tumor’s precise physical and biological traits.
- Predict the outcome of various treatment scenarios and choose the one that best matches the patient’s specific condition.
- Monitor changes in tumor behavior during treatment, allowing for real-time adjustments in the therapy plan.
With these personalized strategies, the tide in cancer care could shift toward more effective, patient-centered therapies. In many ways, this technique embodies the idea of “getting into” the full spectrum of patient needs, where every subtle detail is taken into account in the battle against cancer.
Building Bridges Between Research and Clinical Application
The evolution of 3D bioprinting in the context of cancer research is a prime example of how deep collaboration between academic institutions and medical professionals can lead to groundbreaking discoveries. Researchers, clinicians, and educators are all working together to ensure that the promising innovations in laboratory settings can eventually be integrated into routine clinical practice.
Several key strategies are essential for bridging the gap between experimental success and clinical implementation:
- Interdisciplinary Collaboration: Encouraging joint projects that bring together experts in physics, engineering, biology, and medicine.
- Robust Clinical Trials: Designing and executing studies that carefully evaluate the performance of 3D bioprinted models in real patient scenarios.
- Effective Communication: Facilitating dialogues between research scientists and healthcare practitioners to discuss potential pitfalls and improvements.
These approaches show that while challenges remain—riddled with small problems and tense uncertainties—the dedication and relentless enthusiasm of the research community are central to overcoming them. The promise of more accurate, efficient, and personalized cancer treatment continues to drive progress in this fast-evolving field.
The Broader Impact on Healthcare and Patient Outcomes
The widespread adoption of 3D bioprinting technology in cancer research could lead to a seismic shift in the overall landscape of patient care. Improvements in radiotherapy techniques directly translate into tangible benefits for patients. Not only could such technological advances shorten treatment times, but they might also reduce the side effects that so often accompany conventional therapies.
Several potential benefits for patient care include:
- More Precise Treatments: Custom-tailored radiation doses informed by 3D bioprinted models aim to target tumors more efficiently.
- Enhanced Quality of Life: Minimizing damage to healthy tissues can lead to fewer side effects and better overall wellness during and after treatment.
- Increased Survival Rates: A better understanding of tumor response to varied radiation techniques could pave the way for higher survival rates as treatments become more effective.
The promise of these advances reinforces the significance of investing in innovative research. It also underscores the role that modern technology plays in shaping the future of patient care. By embracing these methods, the medical community not only addresses the immediate challenges of cancer treatment but also lays the groundwork for further innovations that could impact a variety of other complex medical conditions.
Looking Ahead: Future Directions and Ongoing Research
The journey of integrating 3D bioprinting in cancer therapy is only just beginning. Researchers are continuously “diving in” to untangle the multiple layers of tumor biology and test novel hypotheses that could transform treatment paradigms. Future research efforts are expected to explore even more detailed aspects of tumor biomechanics, chemical interactions during radiotherapy, and the potential synergy between radiotherapy and emerging immunotherapies.
Key areas of future investigation include:
- Enhanced Bioprinting Techniques: Further refining printing methods to incorporate even more realistic tissue features, including nerve and immune cell networks.
- Integration with Imaging Technologies: Combining 3D bioprinting with advanced imaging methods to provide real-time feedback during treatment.
- Translational Studies: Moving from bench research to clinical trials that evaluate patient outcomes directly, ensuring that the technology is safely and effectively integrated into standard protocols.
As these research efforts progress, the gap between experimental innovation and routine clinical application will continue to narrow. In doing so, the technology not only promises to “find your way” through the tricky parts of effective cancer treatment but also inspires a new generation of researchers and clinicians committed to continuous improvement in patient care.
Enhancing Communication: The Role of Public Awareness and Education
For the benefits of these innovative techniques to be fully realized, public awareness and education about 3D bioprinting must be enhanced. Bringing the general public, patients, and their families into the conversation is a key step toward a more informed healthcare community. This involves not only explaining the science behind these advances but also addressing the practical implications for treatment options and outcomes.
Educational initiatives can help demystify the sometimes intimidating world of medical physics and bioprinting. Public seminars, interactive workshops, and comprehensive online resources are some of the effective platforms for sharing detailed information. These efforts aim to “get into” the fine points of how modern technology is reshaping cancer treatment while clarifying any confusing bits that may arise.
By increasing awareness, the medical community can offer patients the reassurance that their treatment options are continually evolving toward more precise and effective strategies. In doing so, patients may feel more empowered to engage with their healthcare providers and participate in decision-making regarding their treatment paths.
Patient-Centered Outcomes: A Hopeful Future in Cancer Therapy
The ultimate goal of all these research initiatives is to improve patient outcomes. For those battling cancer, every advancement in treatment techniques is a step toward a brighter future. The application of 3D bioprinted tumor models in optimizing radiotherapy not only enhances treatment precision but also opens up new avenues for personalized care that can be tailored to each patient’s distinct profile.
With personalized treatment plans comes the potential for:
- Fewer Side Effects: More accurate targeting means that healthy tissues are spared from unnecessary radiation exposure.
- Shorter Recovery Times: More efficient treatments can lead to faster recovery, reducing the overall burden on the patient’s body.
- Enhanced Treatment Satisfaction: Patients are likely to feel a greater sense of involvement and confidence when their treatment plans are specifically designed to address their needs.
This patient-centered approach represents a shift away from one-size-fits-all treatment paradigms and moves toward a healthcare model that is truly built around individual needs and conditions. As research continues to mature, the hope is that these technologies will not only extend lives but also enhance the overall well-being of cancer patients.
Reflecting on the Journey: The Intersection of Innovation and Humanity
At its core, the evolution of 3D bioprinted tumor models is a testament to the unyielding human spirit of innovation. It is a journey marked by rigorous scientific inquiry, shared challenges, and a deep commitment to easing the burden of one of the world’s most overwhelming diseases. While the path is strewn with complicated pieces and nerve-racking hurdles, the strides made by researchers are truly inspirational.
This blend of technical advancement and compassionate care serves as a powerful reminder that science is fundamentally a human endeavor. Each experiment and trial represents not only a step forward in our understanding of cancer but also a ray of hope for millions of patients and families facing the reality of the disease.
The ongoing commitment to mentorship, interdisciplinary cooperation, and patient-centered research ensures that the field of medical physics will remain at the forefront of transformative cancer care. It stands as a beacon of how technology and humanity can come together to make significant inroads against one of our most challenging health issues.
Cultivating the Future: The Role of Emerging Technologies in Modern Oncology
The integration of new technologies into oncology is not purely about the technology itself—it is about shaping the future of medicine in a way that is adaptable, empathetic, and incredibly forward-thinking. As researchers continue to fine-tune the methods and applications of 3D bioprinting, the field of radiotherapy will evolve in tandem with these technological advancements.
Emerging tools, such as artificial intelligence and advanced imaging techniques, are expected to work hand-in-hand with bioprinting to identify the most effective treatment protocols. This convergence of technologies will help clinicians “steer through” the challenging landscape of cancer care by offering predictive analytics, real-time treatment monitoring, and pathways to more precise radiation delivery.
Moreover, the rapid advancements brought about by interdisciplinary research encourage a dynamic shift from static treatment models to more interactive and adaptive frameworks. Such frameworks allow for flexible adjustment in treatment strategies based on continuous feedback from both the 3D models and patient outcomes. This iterative process holds great promise for making cancer treatments not only more effective but also more resilient in the face of evolving tumor behaviors.
Charting a Collaborative Path Forward in Oncology Research
Moving forward, the journey from laboratory breakthroughs to comprehensive patient care will heavily rely on collaborative efforts across various disciplines. Researchers, clinicians, educators, and technology experts must come together to ensure that each new discovery is translated into a real-world benefit for patients battling cancer.
This collaborative approach involves:
- Sharing Data and Best Practices: Establishing robust networks where institutions collaboratively share research findings to speed up innovation cycles.
- Cross-Disciplinary Teams: Forming teams that encompass expertise in medical physics, engineering, biology, and clinical practice to solve problems from multiple angles.
- Continued Education and Training: Investing in training programs that equip future generations with the skills and knowledge needed to push these innovations even further.
By pooling resources and expertise, the medical community will be better positioned to overcome any off-putting challenges that arise during the transition from innovative research to everyday clinical application.
A Call for Continued Innovation and Investment in Research
The promise of 3D bioprinting and its application in optimizing radiotherapy for cancer patients is a clear call to action for further investment in research and development. Government bodies, private institutions, and philanthropic organizations all have a role to play in supporting these initiatives.
Investments in technology, infrastructure, and human capital will be super important for sustaining the momentum in these groundbreaking studies. Continued funding can help accelerate clinical trials, drive further technological refinement, and ultimately provide patients with access to the most advanced therapies available.
In summary, the journey toward optimizing cancer treatment through 3D bioprinted tumor models is one filled with both promise and pressing challenges. It also represents a future where the boundary between technological innovation and compassionate care becomes beautifully blurred, forging a path towards more accurate, tailored, and humane cancer therapies.
Conclusion: A Vision for a More Effective and Compassionate Cancer Care Future
The strides made in developing 3D bioprinted tumor models represent much more than a technological breakthrough—they embody hope, resilience, and the relentless pursuit of excellence in cancer treatment. As researchers continue to “dive in” and refine these methods, they are charting a course toward a future where radiotherapy is not only more precise but is also deeply personalized to meet each patient’s unique needs.
This editorial is a call to recognize the impact of interdisciplinary collaboration, technological innovation, and robust mentorship in shaping the future of modern oncology. It sheds light on the promising potential of 3D bioprinting in transforming the way we understand and treat cancer, ensuring that every patient benefits from the most comprehensive, effective, and empathetic care available.
By investing in research that tackles the hidden complexities of tumor biology, healthcare professionals are taking proactive steps to not only extend lives but also enhance the quality of those lives. The integration of these innovative methods into everyday clinical practice is a testament to the power of technology when combined with human ingenuity and compassion.
As we look ahead, the vision remains clear: a future where every cancer patient receives treatment that is finely tuned to the subtle details of their disease, promoting recovery in the most efficient and patient-friendly manner possible. The journey is long and filled with twists and turns, but each new discovery serves as a reminder that together, we can create a more effective, compassionate, and hopeful era in cancer care.
Originally Post From https://www.sdsu.edu/news/2025/10/researchers-use-three-d-bioprinted-tumor
Read more about this topic at
12 new breakthroughs in the fight against cancer
Top Cancer Treatment Advances at MSK in 2024