Reverse Blood Flow Treatment: A Closer Look at Aneurysmal Subarachnoid Hemorrhage in the Setting of Interrupted Aortic Arch
The treatment of aneurysmal subarachnoid hemorrhage (SAH) in patients with rare congenital vascular anomalies—specifically interrupted aortic arch (IAA) combined with an aberrant right subclavian artery (ARSA)—brings forward a range of tricky parts, tangled issues, and subtle details that require us to dig deeper into modern therapeutic methods. Over the years, the evolution of endovascular treatment options has allowed clinicians to find their way through these challenges. In today’s editorial, we will explore the reverse blood flow treatment approach, consider the substantial impact of abnormal hemodynamics, and share insights drawn from a recent case study that has sparked conversation among experts.
With innovations in diagnostics and intervention, more patients with even highly unusual presentations are now provided with safe and effective treatment options. However, managing IAA with ARSA is not without its twists and turns for practitioners who must figure a path through confusing bits and overwhelming anatomical details.
Understanding the Rare Combo: Interrupted Aortic Arch and Aberrant Right Subclavian Artery
At its core, interrupted aortic arch is a rare condition where there is a complete discontinuity between the aortic arch and the descending aorta. It typically presents in infancy with severe cardiac problems, but some patients may develop sufficient collateral circulation to survive into adulthood. While ARSA is a more common variant, burdened with its own set of tricky parts, the merging of these two conditions adds layers of tense interactions to the vascular landscape. Clinicians are forced to get into the nitty-gritty of both defects, analyzing how each abnormality can influence hemodynamic changes and affect the development and rupture of intracranial aneurysms.
Essentially, ARSA occurs when the right subclavian artery arises abnormally, usually from the distal aortic arch or descending aorta. Although this variant is often asymptomatic, in some cases it can cause symptoms such as dysphagia or even lead to complications like aneurysm formation or arterial dissection. When paired with IAA, the potential for erratic blood flow increases, causing damage to the delicate structures of the cerebral vessels, which then may predispose these vessels to aneurysm formation and eventual rupture.
Challenges in Endovascular Approaches for Vascular Anomalies
Interventional treatment in patients with these unusual vascular configurations is often loaded with problems. In traditional setups, clinicians use well-established routes to access the aneurysm site via the femoral or radial arteries. However, in cases where IAA and ARSA coexist, even reaching the target area becomes nerve-racking due to the extreme vessel angles and reverse blood flow phenomena.
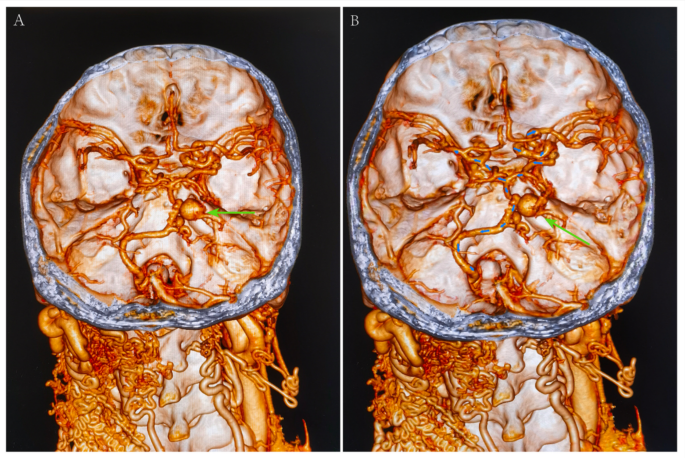
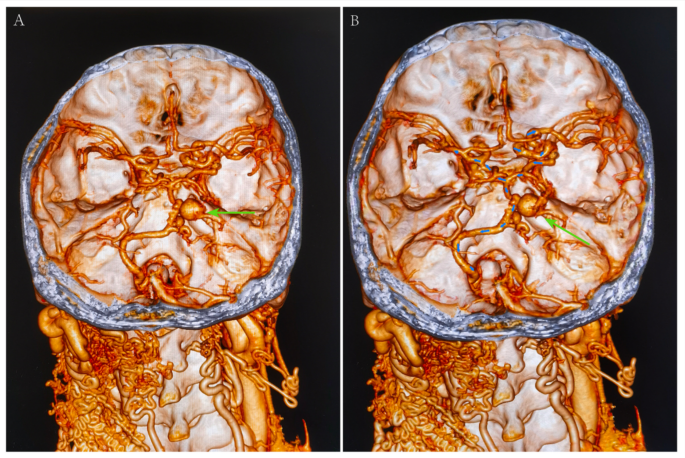
For instance, standard cerebral digital subtraction angiography (DSA) techniques may hit a wall if the guidewire cannot pass the interrupted aortic arch. The reverse flow encountered in the vertebral arteries—owing to compensatory mechanisms—can result in poor visualization of the intracranial vasculature. In such instances, the doctors must figure a path using alternative approaches such as detailed 3D computed tomography angiography (CTA) planning, where every small distinction in the vascular course matters.
Key points to consider in these challenging cases include:
- The unpredictable course of the left vertebral artery.
- Tangled issues related to the reverse blood flow creating a suboptimal roadmap.
- Risky decisions about whether to undertake a direct carotid puncture versus a femoral route.
These considerations emphasize how critical it is for clinicians to work through the small details before proceeding with an intervention, ensuring every possible risk is managed and each step is planned with utmost precision.
Preoperative Imaging: The Key to Unlocking Hidden Complexities
A fundamental aspect of a successful intervention in these scenarios is comprehensive preoperative imaging. With state-of-the-art imaging tools like 3D CTA and digital subtraction angiography, practitioners can take a closer look at the complicated pieces of the vascular structure. These imaging techniques offer a sneak peek into the following fine shades:
- Vessel orientation and branching: Understanding the course of the left vertebral artery and its relationship to the basilar artery is absolutely essential.
- Measurement of aneurysm dimensions: Accurate sizing is crucial to select the right size and number of coils for embolization.
- The angle of access: The preoperative images help determine the best working angles, especially when the catheter’s route is affected by the reverse flow from the vertebral arteries.
These steps allow the clinician to both get into and pinpoint the nitty-gritty of the vascular paths. When planning intervention, cross-sectional imaging provides invaluable details that, despite being subtle, can mean the difference between procedural success and a challenging maze of unexpected complications.
Understanding Hemodynamic Alterations and Aneurysm Formation
Hemodynamics play a key role in the development of intracranial aneurysms. The increased intracranial blood flow, which often results from structural anomalies such as IAA, can act as a double-edged sword. On one hand, it maintains vital blood supply to the brain; on the other, it can be loaded with issues that stress the fragile vessels leading to the formation and possible rupture of an aneurysm.
When the blood pressure proximal to a disruption such as an interrupted aortic arch increases, the stress imposed on the intracranial arterial walls can lead to endothelial cell damage. Consequently, the small details of arterial structure—like the integrity of the internal elastic lamina and the surrounding extracellular matrix—begin to break down. This cumulative damage eventually sets the stage for aneurysm formation.
| Aspect | Description |
|---|---|
| Elevated Pressure | Higher than normal blood pressure in the vessels near the interruption creates additional stress. |
| Collateral Circulation | Alternate pathways form to supply blood which can sometimes result in reverse flow and unusual vector forces in the vessels. |
| Wall Weakening | Continuous abnormal pressure can degrade vessel wall integrity, leading to aneurysm formation. |
| Repair and Remodeling | The body’s attempt to repair these insults may further complicate the normal vascular structure. |
The table above offers an outline of the key hemodynamic components. It highlights how such structural alterations can create a tense environment within the brain’s vascular network, leading to life-threatening events like SAH.
Step-by-Step Insights: The Procedure and Its Twists and Turns
The case study in question showcased a unique approach to managing aneurysmal SAH in a young patient with IAA and ARSA. Here, the intervention strategy required a series of considered steps, each one meticulously planned through preoperative imaging data. The approach was to treat the ruptured aneurysm first with endovascular therapy, followed later by corrective aortic surgery.
Details of the procedure included:
- Initial Challenges: The traditional catheter route through the femoral artery was obstructed by the IAA and ARSA. The team was unable to pass their guidewire through the aortic arch as conventional routes had become ineffective due to reverse blood flow.
- Advanced Imaging Use: By leveraging 3D CTA images, the clinicians identified a suitable path via the left vertebral artery, despite its tortuous and winding nature.
- Endovascular Embolization: With the aneurysmal neck having a favorable shape and minimal width, coil embolization was performed successfully even though the route map was not clearly visible in real-time fluoroscopy.
- Subsequent Aortic Surgery: Once the risk of aneurysm re-rupture was minimized, a careful aortic repair was planned. This procedure notably connected the descending aorta to the left subclavian artery region, essentially re-establishing continuity in the aortic arch.
While these steps may look straightforward on paper, each came with its own set of intimidating fine points and confusing bits. Every decision—from selecting the working angle based on CTA images to opting against a carotid puncture due to a high bleeding risk—required deep consideration and expertise.
Weighing Options: Balancing Endovascular and Surgical Therapies
When managing patients with vascular malformations that are riddled with issues, it is crucial to balance the benefits and risks associated with both endovascular and surgical interventions. Clinicians must carefully assess whether immediate endovascular intervention is the best path forward or whether surgical repair should be prioritized. This decision often depends on:
- The patient’s overall cardiac function
- The extent and degree of collateral circulation
- The potential for intraoperative complications due to reverse blood flow
- The accessibility of the aneurysm through nontraditional entry routes
In the case that we are discussing, the decision to adopt a reverse blood flow management strategy was based on the patient’s robust collateral flow via the internal carotid arteries and the compensatory vessels of the vertebral circulation. The team concluded that a staged approach—starting with the endovascular treatment of the aneurysm and later following up with corrective aortic surgery—provided a safe and effective strategy for long-term neurological preservation.
Stitching the Vascular Puzzle: Preoperative Planning as a Must-Have Step
One of the super important steps in managing such a challenging case is a deep preoperative evaluation and planning process. When clinicians take a closer look at the detailed 3D CTA images, they are essentially piecing together a complex vascular puzzle. Every subtle detail – such as the diameter of the vessel, the orientation of the aneurysm, and even the tiny twists in the arterial course – must be understood before going ahead with any intervention.
Key advantages of thorough preoperative planning include:
- Reduced Risk: By mapping out the vascular routes ahead of time, the risks associated with unexpected bleeding or catheter misplacement are minimized.
- Optimized Outcome: Detailed knowledge of the vascular map leads to better coil placement and more effective embolization of the aneurysm.
- Tailored Intervention: Understanding the unique vascular layout allows a custom treatment plan that accounts for every fine shade of the patient’s anatomy.
These steps are critical as they offer the surgical team insights that help them steer through each stage of the treatment, especially when confronted with tangled blood flow dynamics and challenging vascular access points.
Postoperative Follow-Up: Assessing the Long-Term Impact
Following the complex procedures, long-term follow-up has proven essential in understanding the success rate and potential late-onset complications in patients undergoing such interventions. Regular monitoring using digital subtraction angiography (DSA) and computed tomography angiography (CTA) has revealed a remarkable reconstruction of the vascular network in the case we reviewed.
For instance:
- The disappearance of multiple intracranial aneurysms was noted in follow-up imaging, underlining the role of hemodynamic improvement following surgical correction of the aortic defect.
- The maintenance of the coil embolization within the aneurysm, which continued to prevent re-rupture, was an encouraging sign of procedural success.
- The observed improvement in collateral circulation, particularly the enhanced visibility of the left vertebral artery post-surgery, provided objective evidence of improved hemodynamics.
These follow-up studies are key. They not only affirm the immediate benefits but also help in anticipating long-term outcomes, ensuring patients remain well and symptom-free even many years after their initial interventions.
Innovative Strategies: Learning from the Case to Improve Future Treatments
This case study serves as an important lesson in the application of innovative strategies to manage complex vascular scenarios. It highlights that even when faced with a vascular maze loaded with issues—ranging from unpredictable blood flow to difficult vessel access—detailed planning and individualized treatment approaches can result in favourable outcomes.
Based on the experience gleaned from this patient’s care, here are several takeaways for healthcare practitioners:
- Individualized Assessment: Always perform a thorough evaluation of the patient’s specific vascular pattern before deciding on the treatment strategy.
- Prioritize Safety: Opt for less invasive endovascular techniques when open surgery carries high risks due to anatomical constraints.
- Adaptability: Be prepared to adapt your approach when conventional routes fail – for example, by switching from a direct carotid puncture to a femoral approach when intraoperative imaging reveals hidden twists and turns.
- Continuous Monitoring: Regular follow-up imaging should be an integral part of the treatment plan to detect any delayed complications or further vascular changes.
Implementing these strategies not only improves immediate treatment outcomes but also enhances our overall understanding of how abnormal vascular dynamics evolve over time. It prompts practitioners to get into the science of hemodynamics and the subtle interplay between structural abnormalities and vascular health, fostering a more holistic approach to patient care.
Exploring Alternative Medical Perspectives in Vascular Treatment
There is also a growing interest in alternative perspectives when it comes to managing patients with unusual vascular conditions. Many experts have started to consider whether complementary therapies and lifestyle changes might help modulate some of the hemodynamic stress seen in these patients. In cases where high blood pressure is a contributing factor, integrating nutritional advice, yoga, and meditation might have a supportive role alongside medical interventions.
While such methods do not replace definitive surgical or endovascular treatment, they can serve as a springboard for patients to manage their overall cardiovascular health. The integration of modern interventional techniques with complementary lifestyle strategies reflects a broader shift in medical practice – one that privileges a well-rounded, patient-centric approach to treatment.
Key Observations: Summarizing the Findings
To wrap up our discussion, it is useful to summarize the key points that have emerged from our analysis of the reverse blood flow treatment strategy in the context of IAA coupled with ARSA:
- Understanding Rare Anatomies: The combination of IAA and ARSA presents multiple tricky parts that require careful imaging and preoperative planning.
- Impact of Hemodynamics: Abnormal blood flow is a critical factor in the formation of intracranial aneurysms. Improved collateral circulation post-surgery can mitigate these issues.
- Planning and Adaptability: Success hinges on a detailed understanding of the small distinctions in vascular anatomy. Working through these challenging details helps clinicians decide on the optimal interventional route.
- Endovascular Versatility: Even in the presence of overwhelming anatomical constraints, tailoring the approach and utilizing advanced imaging techniques can lead to safe and effective aneurysm obliteration.
- Long-Term Follow-Up: Regular imaging and monitoring after the procedure provide evidence of success and guide further management in complex cases.
Each of these elements demonstrates that while the management of vascular anomalies may be loaded with issues and intimidating twists, a careful, patient-specific approach can yield highly satisfactory outcomes.
Looking Ahead: The Future of Vascular Intervention in Complex Cases
In our rapidly advancing medical era, the future looks promising for patients with complex vascular anomalies. As cutting-edge imaging techniques and innovative interventional tools continue to evolve, clinicians can now manage even the most challenging vascular conditions with improved precision. Going forward, the integration of computer-assisted planning and augmented reality may help practitioners steer through the minute details of vascular anatomy in real-time, making procedures even more effective and safe.
Areas of potential future innovation include:
- Enhanced Imaging Software: Programs that allow for ultra-high-resolution 3D modeling could make it even easier to pinpoint every small distinction that affects blood flow directions inside the brain.
- Robotic-Assisted Endovascular Navigation: Automation in catheter placement could reduce operator error and help manage the complex pieces of vascular anatomy more efficiently.
- Biomaterial Advances: Improved embolic materials that adapt to the vessel’s shape may enhance the long-term durability of aneurysm treatment.
- Personalized Medicine: Tailored treatment protocols based on the genetic and molecular profiles of the patient might one day contribute to better prevention strategies for aneurysm formation in patients with congenital vascular anomalies.
These advancements will not only improve procedural success rates but also help reduce the post-treatment complications associated with altered hemodynamics. The lessons learned from managing aortic arch discontinuities and aberrant vessels will pave the way for more holistic and innovative treatment techniques in the near future.
Final Thoughts: Balancing Innovation and Patient Safety
The journey of treating aneurysmal subarachnoid hemorrhage in patients with IAA and ARSA reminds us that medicine is as much an art as it is a science. Every patient presents a unique set of challenges—from nerve-racking reverse flows to the complicated twists and turns of collateral circulation. The successful case we discussed demonstrates that with precise imaging, careful planning, and an adaptable treatment strategy, even the most tense vascular puzzles can be solved.
While the medical community continues to search for more refined techniques and technological improvements, patient safety remains the ultimate priority. Clinicians must maintain a balanced approach, integrating state-of-the-art endovascular therapies with scheduled follow-ups and supportive lifestyle measures. In doing so, they not only manage the immediate threats posed by aneurysm rupture but also work to prevent further complications by addressing the underlying hemodynamic disturbances.
In essence, this case reinforces that a detailed understanding of vascular anatomy and hemodynamics is essential for success. The reverse blood flow treatment represents an important example of how innovation, when combined with rigorous planning, can effectively untangle even the most confusing and intimidating vascular issues. As we continue to work through the subtle parts and hidden complexities, every advancement contributes to safer, more tailored care for patients with these rare but challenging vascular conditions.
Summary and Clinical Takeaways
In summary, tackling the reverse blood flow treatment for SAH in patients with IAA and ARSA requires:
- In-depth preoperative imaging to map out every fine point and subtle twist in the vascular structure.
- A flexible, stepwise approach that initially focuses on stabilizing life-threatening aneurysmal rupture before addressing the structural heart anomaly.
- Careful evaluation of the impact of reverse blood flow on catheter navigation and aneurysm visualization.
- Long-term postoperative monitoring to ensure that the reconstructed aortic arch and associated collateral vessels continue to function optimally.
These clinical takeaways not only improve our current practice but also pave the way for future research and technical enhancements. They remind us that even when faced with overwhelming challenges, the combination of detailed planning, innovative technology, and a balanced treatment strategy can lead to successful patient outcomes.
Conclusion
The management of aneurysmal SAH in the context of IAA and ARSA is undeniably loaded with challenging twists and nerve-racking obstacles. However, as this case study reveals, a thoughtful and well-planned approach based on advanced imaging and tailored endovascular intervention can lead to excellent long-term outcomes. By taking the time to figure a path through the confusing bits of abnormal hemodynamics, vascular specialists can deliver treatments that not only address the immediate threat of aneurysm rupture but also improve overall cerebral perfusion and patient quality of life.
Looking beyond this single case, it is clear that ongoing collaboration between interventional radiologists, neurosurgeons, and cardiac surgeons will be super important. The integration of modern imaging, robotic assistance, and innovative embolic materials holds promise in enhancing the safety and precision of interventions in patients with vascular anomalies. Ultimately, balancing innovation with patient safety will remain the cornerstone of effective healthcare delivery in the ever-evolving world of vascular medicine.
As we continue to work together and learn from each complicated piece and subtle part along the way, the future is bright for patients and practitioners alike. The lessons learned from such pioneering cases serve as stepping stones on the path to improved treatment algorithms and refined surgical techniques—ensuring that even the most nerve-racking cases can be managed with confidence and expertise.
Originally Post From https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-025-04466-0
Read more about this topic at
A Comprehensive Approach to Middle Cerebral Artery …
Navigating Complex Vascular Pathways With “Meet in the …