Childhood Obesity and Early Vascular Injury: A Closer Look at Emerging Evidence
The latest research published in the International Journal of Obesity sheds new light on the connection between childhood obesity and early vascular injury. In this opinion editorial, we take a closer look at the study led by Thomazini et al., which suggests that excess weight in children may be linked to blood vessel damage at an early age. The findings have raised concerns about long-term cardiovascular risks, and they urge us to consider preventive measures before the situation worsens.
Understanding the study’s premise can be a bit intimidating at first glance, especially given the tricky parts involved in teasing apart the causes and effects. However, a deeper exploration of the evidence reveals some key insights into how early obesity may set young bodies on a path toward chronic cardiovascular issues. This editorial delves into the small distinctions between healthy vascular function and the subtle signs of injury observed in children who are overweight.
Early Vascular Stress in Pediatric Populations: Observations and Implications
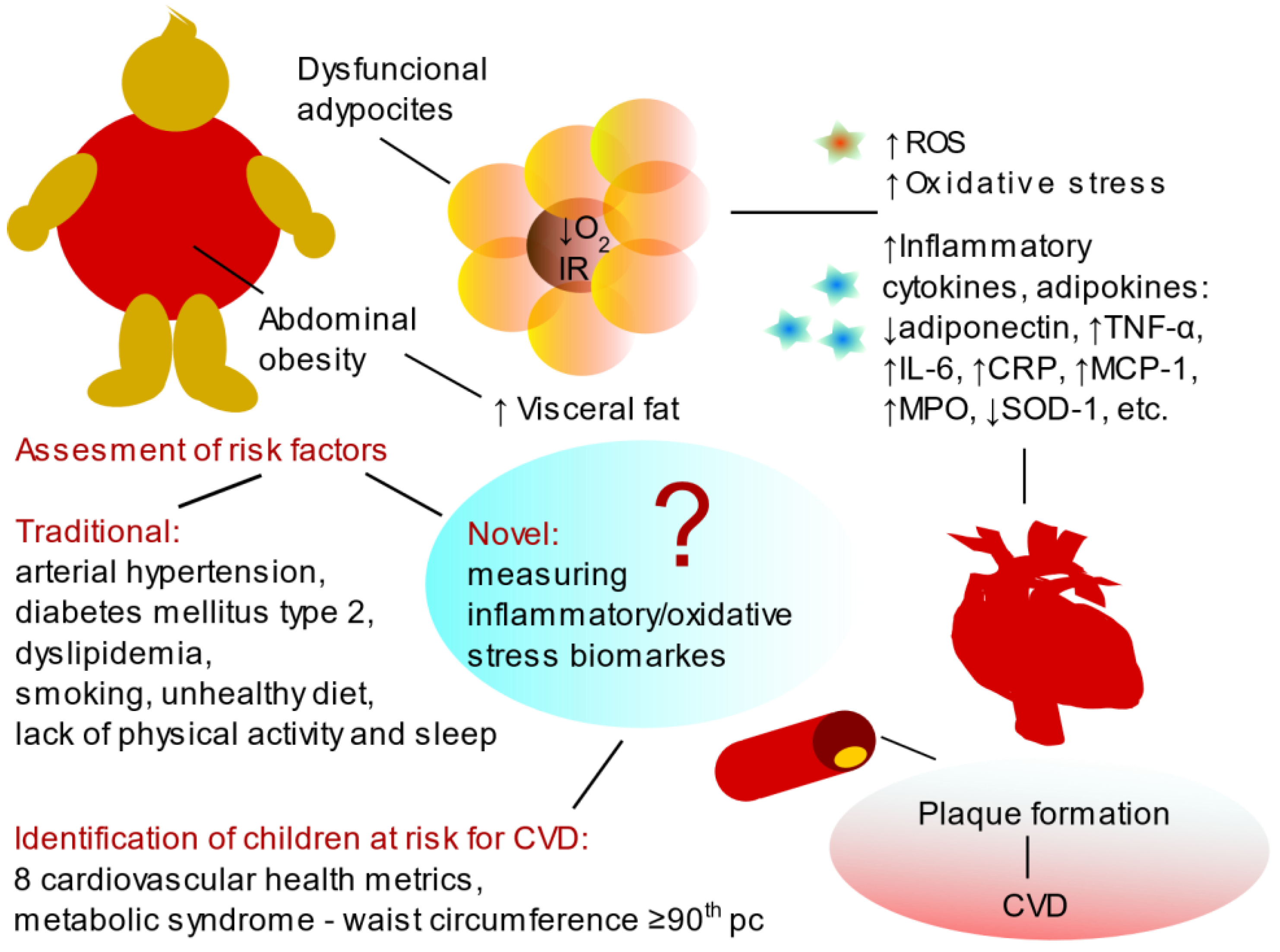
One of the central topics of the study revolves around the idea that obesity in children might trigger early signs of vascular damage. Researchers have noted changes in the markers of vascular health among obese children, which could indicate that their blood vessels are under stress. These findings point to a scenario where the little details of vascular function shift in the presence of excess fat, even before any overt cardiovascular disease appears.
When we get into the nitty-gritty of the study, we see that the blood vessels of obese children show signs of injury or stress. These early vascular changes may include reduced vessel elasticity, abnormal inflammatory markers, and other markers of stress that, while not immediately life-threatening, might have serious implications as the child grows older. It is a reminder that the different twists and turns in how the body manages extra weight can have long-lasting effects.
Experts argue that the results emphasize the critical need to spot these subtle parts early and to adopt strategies that can mitigate future cardiovascular complications. The study suggests that pediatric obesity has consequences not only on a child’s immediate physical well-being but also on their future heart health. Given the overlap between the obvious physical manifestations of obesity and the hidden issues in blood vessel health, our approach to tackling these problems must be both comprehensive and proactive.
Pediatric Cardiovascular Risk Assessment: Riddled with Issues or Loaded with Opportunities?
Assessing cardiovascular risks in children presents its own set of tricky challenges. Over the years, medical professionals have focused on adult populations when looking at heart disease. However, this study paves the way to better understand early vascular injury in a younger demographic. By recognizing the early vascular signs among obese children, clinicians have the chance to figure a path toward early intervention, thereby limiting future cardiac complications.
Historically, the diagnostic criteria for detecting vascular injury have been tailored for adults. The findings from Thomazini et al. remind us that young bodies can also exhibit early signs of risk. Some of the challenging bits include finding age-appropriate, non-invasive ways to monitor vascular health in children. Breaking down the complicated pieces of cardiovascular risk assessment in pediatric patients might involve redesigned screening protocols that capture the fine points of early vascular stress.
There is a growing consensus among pediatric cardiovascular specialists that early prevention is super important. A multi-tiered approach – including regular health check-ups, improved diet, and increased physical activity – could all play a role in curbing the onset of early vascular damage. The long-term potential benefits of such interventions make the task of sorting out these issues a must-have priority for healthcare providers and parents alike.
Preventative Strategies: Tackling the Hidden Complexities of Childhood Obesity
Addressing childhood obesity is not simply about reducing the numbers on a scale; it is about taking care of the whole organism, including the hidden complexities of vascular health. With the alarming evidence that obesity might contribute to early arterial damage, a multi-faceted approach becomes essential.
Many strategies can be considered to manage a child’s weight and improve their overall cardiovascular health. Educational initiatives, community programs, and family-centered interventions can all help steer through the tricky parts of intervention. The goal is to get around the early indicators of vascular stress and nip potential long-term complications in the bud.
- Nutrition Education: Teaching children and parents about balanced diets and the importance of portion control.
- Physical Activity Programs: Incorporating fun, engaging exercise routines that can be integrated into daily life.
- Routine Vascular Health Screenings: Implementing teen-friendly assessments to monitor blood vessel health over time.
- Community Engagement: Creating community spaces that encourage outdoor activities and healthy lifestyles.
Each of these strategies requires more than just a quick fix. It means taking a deeper look into the factors that contribute to weight gain and poor vascular health, as well as addressing the socio-economic and emotional factors that can exacerbate these issues. In many ways, the fight against childhood obesity is as much about education and community as it is about medical intervention.
Understanding the Tricky Parts of Vascular Health in Young Bodies
Young bodies are dynamic systems that are still developing. The vascular system, in particular, is subject to many of the same influences that affect overall weight. Increased body fat can lead to a state of chronic inflammation, which in turn might result in stiffening of the arteries or subtle injuries to the blood vessel walls. These changes may initially be slight, but over time they can set the stage for more serious cardiovascular problems.
What is particularly noteworthy about this study is that these changes are not limited to individuals with long-term obesity. Even relatively recent increases in weight can trigger changes in the vascular system. This suggests that the early stages of obesity – perhaps even before an individual is considered clinically obese – might already be setting up the body for future complications.
For families and practitioners, this raises a series of important questions: How early should vascular health be assessed? Should there be routine non-invasive screenings in schools or pediatric visits? And importantly, what role can early lifestyle changes play in reversing or halting these changes?
The Role of Lifestyle Modification in Mitigating Early Vascular Damage
One of the most effective measures that can be taken is lifestyle modification. When it comes to managing childhood obesity and its complications, getting into healthier eating habits and encouraging active living are key. While the study points to measurable vascular changes in obese children, there is growing evidence that these changes can be reversed or mitigated through concerted efforts on diet and exercise.
It is essential for parents, educators, and healthcare providers to work together to craft environments where healthy choices become the norm rather than the exception. Some practical suggestions include:
- Home-Cooked Meals: Prioritize meals that are nutrient-dense and low in processed ingredients.
- Active Playtime: Regular outdoor play can help maintain an active lifestyle and reduce sedentary behaviors.
- Health-Centered School Programs: Schools adopting comprehensive physical education routines can contribute significantly to overall health.
- Mindful Eating Practices: Educating children on recognizing hunger signals and avoiding overeating.
When communities take the wheel in fostering healthier lifestyles, children are more likely to adopt habits that steer them away from the risky route of long-term cardiovascular diseases. Health and socioeconomic policies that subsidize healthy foods and provide safe exercise facilities are part of a broader system that supports these lifestyle choices.
Socio-Economic Factors and Childhood Obesity: A Multifaceted Issue
The issue of childhood obesity and its associated risks is not isolated from the socio-economic context in which a child lives. Income disparities, access to education, and availability of healthy foods play a critical role in shaping a child’s lifestyle. In communities where resources are limited, challenges can be even more overwhelming.
While it may be nerve-racking to confront these twisted issues, understanding them is the first step toward effective intervention. Research has shown that children in lower-income areas may be exposed to fewer fresh food options and fewer safe spaces for physical activity, increasing the likelihood of obesity and subsequent early vascular injury.
Addressing these socio-economic factors requires a multi-pronged approach:
- Policy Measures: Governments can implement policies to subsidize healthy food options and incentivize grocery stores to open in underserved areas.
- Public Health Programs: Local public health initiatives can provide nutrition and physical activity resources to families who need them the most.
- Community Engagement: Partnerships with non-profit organizations, schools, and local businesses can foster community gardens and safe play zones.
- Education and Awareness: Targeted campaigns to educate communities about the link between obesity and cardiovascular health.
By addressing these facets head-on, we enable a more robust, community-level response that not only treats the symptoms of childhood obesity but also works to eradicate its roots. It is a reminder that when tackling such a full-of-problems issue, there is no one-size-fits-all solution – each community must find its own way through the tangled issues.
Navigating the Challenging Bits: A Comprehensive Approach to Prevention
When it comes to preventing long-term cardiovascular issues, it is important that efforts are holistic and well-coordinated. The potential for significant vascular instability in obese children cannot be ignored, and the onus falls on both healthcare providers and societies to work together on this front.
A comprehensive approach involves not only medical intervention but also educational and community policy changes. By adopting routine screenings for vascular health in children, healthcare providers can identify early signs of injury and provide targeted interventions. This requires a shift in traditional practices, encouraging doctors to pay attention to the early signals of vascular stress that may be overshadowed by more visible symptoms of obesity.
The following table summarizes some key steps that can help manage early vascular injury in obese children:
| Strategy | Action Steps | Expected Benefits |
|---|---|---|
| Regular Health Screenings |
|
|
| Diet and Nutrition |
|
|
| Physical Activity |
|
|
| Community and Educational Programs |
|
|
Each strategy listed in the table above demands a detailed, multi-disciplinary approach in order to be successful. When efforts are synchronized between public health policies, clinical practices, and community initiatives, the potential to mitigate early vascular damage becomes more tangible.
The Importance of Early Intervention and Long-Term Monitoring
The evidence gathered by Thomazini et al. points squarely to the need for early intervention. As the early vascular indicators in obese children are only just beginning to manifest, taking the time to manage these issues now is super important in preventing more severe cardiovascular complications later in life.
Early intervention has many advantages. Not only can it help reduce immediate health problems, but it also sets the stage for healthier future outcomes. Healthcare providers should work to integrate vascular monitoring as part of routine check-ups, especially in communities where obesity rates are high. Such foresight can reduce the nerve-racking probability of encountering serious cardiovascular events in adulthood.
Long-term monitoring will also ensure that any improvements are maintained. Tracking subtle details like improvements in arterial flexibility and inflammation levels provides tangible measures of success. It also helps identify which interventions are working best, allowing for adjustments in care plans as needed.
The Role of Alternative Medicine and Nutritional Interventions
While traditional medical approaches remain critical, alternative medicine and nutritional strategies also have a part to play in the comprehensive care of obese children. Many families are beginning to ask questions about herbal supplements, mindfulness practices, and unique dietary regimens that can complement conventional treatments.
Alternative therapies do not replace standard treatments, but they can help manage the overall condition when used in tandem with medical care. Some complementary strategies include:
- Herbal Supplements: Certain herbs have been suggested to have anti-inflammatory effects, potentially lowering the markers that indicate vascular stress.
- Mindfulness and Stress Reduction: Techniques such as meditation and yoga may improve overall well-being, indirectly benefiting heart health.
- Customized Nutrition Plans: Diets that emphasize whole, minimally processed foods can support a healthy metabolism and reduce inflammation.
- Physical Therapies: Practices like acupuncture and massage therapy may help reduce bodily stress and promote recovery.
It is paramount that parents and caregivers discuss any alternative treatment ideas with their healthcare professionals to ensure they complement the overall treatment plan. The combination of traditional and alternative approaches can often smooth the twisted journey toward better health.
Policy Implications and the Need for a Community-Focused Approach
The emerging connection between childhood obesity and early vascular injury is not just a matter for clinicians—it’s a community issue. Strategies that target this problem must be supported by well-crafted policies at the local, state, and national levels. Public health officials, policymakers, and community leaders need to prioritize initiatives that address the root causes of obesity.
There are several policy-related areas that need further development:
- Access to Healthy Foods: Policies that encourage the establishment of local markets and reduce the cost of fresh produce can make a dramatic difference in community health.
- Urban Planning Initiatives: Designing communities that prioritize safe walking and biking paths, parks, and recreational facilities can encourage families to get outdoors more often.
- Health Education Programs: School-based and community programs that focus on nutrition, exercise, and the dangers of obesity can empower families to take proactive steps.
- Healthcare Access: Ensuring that preventive care, including routine screenings and follow-up care, is accessible to all segments of the population is essential.
When policy measures are aligned with the needs of the community, every stakeholder—be it students, parents, or healthcare providers—can work together toward the common goal of reducing the incidence of childhood obesity and its long-term complications. With policy in place, communities can overcome some of the overwhelming odds by designing environments that naturally promote healthier lifestyles.
Challenges in the Real World: Facing the Tangled Issues Head-On
Despite the advances in our understanding, the road ahead is not free of obstacles. Families dealing with childhood obesity acknowledge that the twists and turns of making significant lifestyle choices can be overwhelming. Changing nutritional habits, increasing physical activity, and maintaining consistent medical oversight are all tasks that demand dedicated effort and perseverance.
Here are several of the most intimidating hurdles families may encounter:
- Economic Barriers: Limited financial resources can restrict access to healthy food options and recreational activities.
- Time Constraints: Busy family schedules can make it challenging to prioritize home-cooked meals or regular exercise.
- Cultural Expectations: In some communities, traditional dietary habits may be high in calories and low in nutritional value, adding a layer of complexity to dietary changes.
- Lack of Awareness: Without proper education on the early signs of vascular injury, many families might not realize the urgency of the issue until complications arise.
Addressing these obstacles requires a consolidated effort between families, schools, healthcare providers, and government bodies. Working together means sharing the workload and finding creative solutions to untangle these issues. The collaboration between multiple sectors of society is a key ingredient in ensuring that the burden does not fall solely on families already burdened by various pressures.
Looking Ahead: A Future Where Early Intervention Saves Lives
The evidence is clear: childhood obesity can lead to early vascular injury, which in turn sets the stage for long-term cardiovascular risks. With the increasing prevalence of obesity in younger populations, there’s an urgent need to take proactive steps to protect children’s health. The study by Thomazini et al. should serve as a wake-up call to parents, educators, and healthcare professionals alike.
When the small distinctions in a child’s vascular health are recognized early, it opens up a window of opportunity for preventive actions. Future research should continue to explore these early indicators, while policy measures and community programs work in tandem to support families. In addition, adopting and integrating alternative medicine strategies and nutritional interventions may offer a more well-rounded approach to combating obesity.
In closing, while childhood obesity and its related vascular problems present a tangled issue filled with challenging bits and nerve-racking obstacles, they also offer a unique opportunity: the chance to intervene early and change a child’s health trajectory for the better. By working collectively—through improved healthcare strategies, socioeconomic interventions, and supportive policies—the future might just shine a little brighter for the next generation.
Key Takeaways for Parents and Healthcare Providers
In summary, here are some essential bullet points to remember when tackling the issue of childhood obesity and early vascular injury:
- Recognize early signs: Even subtle changes in vascular health can be an indication of future problems.
- Focus on prevention: Early intervention is key to thwarting long-term cardiovascular risks.
- Promote healthy lifestyles: Balanced nutrition, regular exercise, and educational support can make a big difference.
- Advocate for policies: Support community and governmental initiatives that improve access to healthy food and safe recreational spaces.
- Consider all options: Traditional medicine, complemented by alternative therapies, can provide a holistic approach to wellness.
By keeping these points in mind, both parents and healthcare providers can work collaboratively to get around the overwhelming challenges and encourage a healthier future for our children.
Conclusion: A Call to Action for a Healthier Tomorrow
Childhood obesity is not merely a current health issue—it is a precursor to potentially serious cardiovascular problems later in life. Emerging research linking early vascular injury to obesity in children should serve as a clarion call for all stakeholders to act. Even though the journey through the confusing bits and overwhelming challenges of addressing childhood obesity is loaded with problems, the benefits of early intervention cannot be overstated.
With a coordinated effort that includes family education, community support, policy changes, and regular medical screening, it is possible to divert from the dangerous path that early vascular injury sets. The responsibility rests on us all—to steer through the tangled issues and to create an environment that nurtures healthier lifestyles, starting from childhood.
By taking even small steps today, we can ensure that the fine shades of future heart health are painted with care and attention. Understanding that every positive change counts is the first stride toward a clearer, healthier future for our children. It is a shared mission that calls for commitment, collaboration, and continuous curiosity about the long-term effects of today’s lifestyle choices on tomorrow’s health.
Ultimately, this research and ongoing dialogues among health professionals, communities, and policymakers provide a roadmap to manage and mitigate the adverse effects of childhood obesity. We must dig into these challenges with unwavering determination and work together to create a future where early vascular injury is a chapter in the past rather than a looming threat in the future.
Originally Post From https://www.geneonline.com/study-links-childhood-obesity-to-early-vascular-injury-and-cardiovascular-risks/
Read more about this topic at
A Basic Introduction to Pediatric Vascular Anomalies – PMC
Vascular Anomalies
