Opinion: Innovations in Rotational Atherectomy Procedures Could Improve Patient Outcomes
The field of interventional cardiology has seen significant advances over the past decades, and one area that continues to generate buzz is the treatment of moderate-to-severe calcified coronary lesions. In particular, the evolution of rotational atherectomy (RA) techniques has drawn attention for its potential to reduce myocardial injury. A recent study compared the use of low-temperature RA-flush solution with the traditional room-temperature solution. The findings suggest that subtle changes in the procedure might help reduce complications—a topic that is both intriguing and essential for healthcare professionals and patients alike.
Understanding the Role of Rotational Atherectomy in Percutaneous Coronary Intervention
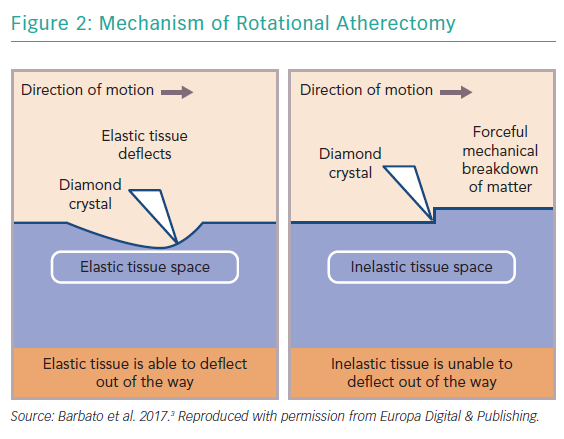
Rotational atherectomy has been a mainstay in the treatment of calcified coronary lesions for over 30 years. Despite its long history, the procedure remains loaded with tricky parts and confusing bits, especially when dealing with calcified plaques where the device must effectively debulk hard tissue without injuring the surrounding structures. This therapeutic method involves a high-speed rotating burr designed to ablate calcified deposits that can obstruct blood flow. However, the procedure itself carries inherent risks that are on edge with issues like myocardial injury, transient slow or no flow, and coronary spasms.
The Cooling Concept: Why Temperature Matters
The key innovation discussed in the recent study is the use of a low-temperature RA-flush solution. Essentially, while the traditional RA approach uses room-temperature solution to continuously flush and cool the moving burr, this new protocol involves storing the flush solution at 0–5°C, thereby providing additional cooling effects during the procedure.
Why is this cooling important? Some of the little details include:
- Heat Generation: The friction between the rapidly rotating burr and calcified lesions generates significant heat. This heat can damage the local myocardial tissue—a phenomenon sometimes described as local thermal tissue damage.
- Debris Embolization: The abrasive nature of RA results in debris that can block small coronary vessels, leading to slow or no flow. Cooler solutions might better manage this risk by reducing the local temperature and the resulting inflammation.
- Myocardial Injury: Elevated levels of cardiac biomarkers, such as cardiac troponin I (cTnI) and creatine kinase isoenzyme (CK-MB), are clinical indicators of myocardial injury. The study found fewer occurrences of these elevations with the low-temperature approach.
A Closer Look at the Study’s Findings
In the multicenter randomized study, 132 patients undergoing RA for the treatment of calcified coronary artery lesions were divided into two groups. One group received the low-temperature RA-flush solution, and the other continued with the room-temperature solution. After the procedure, the patient outcomes were analyzed by measuring peaks in myocardial biomarkers over a 72-hour period.
The results were notable:
- Reduced Myocardial Injury: Patients treated with the low-temperature solution experienced significantly lower rates of myocardial injury (47.0% vs. 71.2% when measured by cTnI, and 28.8% vs. 62.1% when measured by CK-MB) compared to those who received room-temperature solution.
- Fewer Coronary Spasms and Flow Issues: The low-temperature group had lower incidents of transient slow/no flow (6.1% vs. 34.8%) and transient coronary spasm (9.1% vs. 25.8%).
- Comparable Procedural Success: Although the cooling solution improved some aspects of the procedure, there was no significant difference in the overall outcomes such as the incidence of RA-related myocardial infarction or long-term outcomes like target vessel failure at one-year follow-up.
Examining the Cooling Mechanism: A Deeper Dive
At the heart of this innovation is the idea that even a subtle change in temperature during the procedure can influence outcomes. We can break down the cooling mechanism into several critical aspects:
How Cooling Affects Burr Heat Generation
The high-speed rotation of the burr inevitably produces heat. In many procedures, the cooling effect of the flush solution, when used at room temperature, is sometimes not enough to counteract the friction-induced thermal spikes. By cooling the solution down to around 2°C initially and maintaining a lower final temperature than the conventional method, clinicians can help manage the heat generation more effectively. This slight cooling not only protects the tissue but also might stabilize the speed of the burr. Less speed deceleration translates to less abrupt temperature spikes, which is an essential factor in reducing local thermal injury.
Impact on Microcirculatory Blood Flow
Local hypothermia created by the low-temperature flush solution appears to have a two-fold benefit. First, it cools the target coronary segment, possibly reducing myocardial oxygen demand during the intervention. Second, it may limit the inflammatory cascade that can occur after the introduction of debris and heat, thereby reducing the likelihood of transient slow or no flow phenomena.
A simplified table below illustrates the comparison between the two approaches:
| Parameter | Room-Temperature Solution | Low-Temperature Solution |
|---|---|---|
| Initial Flush Temperature | ~22.6°C | ~2.1°C |
| Final Flush Temperature | ~22.9°C | ~6.1°C |
| Transient Slow/No Flow Incidence | 34.8% | 6.1% |
| Transient Coronary Spasm Incidence | 25.8% | 9.1% |
Considering the Broader Implications for Clinical Practice
When we take a closer look at the study’s findings and the mechanism behind the cooling effect, several points come to the forefront that clinicians and researchers might want to consider:
Reducing Risks During RA Procedures
The direct comparison between low-temperature and room-temperature solutions indicates that simple modifications in the procedural environment can have a measurable impact. While the RA procedure itself is effective for modifying calcified lesions, the overall process is loaded with tricky parts that can lead to complications. By reducing local thermal damage through improved cooling, the method shows a promising way to minimize myocardial injury during an already challenging procedure.
The Balance Between Procedural Efficiency and Patient Safety
One of the most compelling arguments for adopting the low-temperature flush solution is the balance between efficacy and safety. Although the procedure’s end goal—successful lesion modification and stenting—remains unchanged, the process benefits from being more patient-friendly by reducing the side effects related to procedural heat and its consequences. This might empower interventional cardiologists to achieve better outcomes with fewer nerve-racking complications.
Long-Term Outcomes and the Need for Further Research
Despite the noticeable improvements in immediate myocardial protection with low-temperature RA solutions, long-term outcomes such as target vessel revascularization and overall patient survival appear to be similar between the two groups. This highlights the need for additional studies to understand whether the benefits of reducing myocardial injury in the immediate period translate to a lower incidence of long-term complications. Here are a few questions that still need answering:
- Will the reduction in myocardial injury lead to a decrease in long-term heart failure or arrhythmias?
- Could the low-temperature approach be optimized further by adjusting the burr-to-vessel size ratio or other procedural details?
- Are there any downsides or risks associated with the use of very cold solutions, such as potential vessel spasm in sensitive patients?
Addressing the Tricky Parts: Potential Limitations and Considerations
While the study offers promising insights into the benefits of using a low-temperature RA-flush solution, several subtle parts and competing factors must be considered before this technique is widely adopted.
Distinguishing RA-Related Injury from General PCI Damage
One of the challenges faced in studies like this is adequately attributing myocardial injury specifically to the RA procedure. In real-world clinical practice, many factors contribute to biomarker elevations following percutaneous coronary intervention (PCI). For instance, phenomena such as distal embolization, microvascular injury, or underlying myocardial conditions can all elevate cTnI and CK-MB independently from the RA procedure. This makes it difficult to be entirely certain that the measured reduction in biomarkers is solely due to the difference in flush solution temperatures.
The Role of Patient Selection and Procedure Planning
The study was conducted on a well-selected patient population with moderate-to-severe calcified lesions that required RA prior to stent implantation. It is essential to note that not all patients undergoing PCI will have lesions that are so calcified that they demand rotational atherectomy. Therefore, when considering the broader application of these findings, clinicians must be cautious. It is important to steer through the patient selection process and to ensure that the benefits of the cooling method outweigh any potential risks, particularly in patients with multiple co-morbidities or those undergoing unplanned RA procedures.
Operational Considerations and Practical Issues
The implementation of a low-temperature RA-flush solution approach may require some adjustments in the catheterization lab. For example, storing and consistently maintaining the saline solution at the target low temperatures could pose logistic challenges. The benefits of this change may justify the extra steps, but it is crucial to iron out these details before large-scale adoption. Consider these operational tips:
- Ensure that the flush solution is stored in a dedicated refrigerator maintained at 0–5°C.
- Monitor the temperature of the solution just before and after the procedure to ensure consistency.
- Train cath lab staff on the revised protocols to avoid any mix-ups between room-temperature and low-temperature solutions.
Reactions from the Interventional Community
Many in the field of interventional cardiology find the idea of using a low-temperature flush solution to be an ingenious yet straightforward modification. Given that RA procedures are already known for their nerve-racking twists and turns, any tactic that can reduce the chance of complications is likely to gain quick acceptance. However, the community remains cautious due to the limited data on long-term outcomes and the need for replication in larger studies.
Expert Opinions and Future Directions
Experts suggest that the critical factor will be validating these early findings in more extensive, possibly multicenter studies that include a broader array of patient presentations. Some clinicians believe that the following points are key to further optimizing RA outcomes:
- Personalized Medicine: Tailoring the temperature and composition of the flush solution to the patient’s specific physiological conditions could enhance safety even further.
- Integration with Other Techniques: Combining low-temperature RA-flush approaches with advanced imaging technologies may help reduce the already complicated pieces associated with procedural planning.
- Continuous Education: Ensuring that interventional teams stay updated on the subtle details of new protocols is essential for safe and effective implementation.
Comparing with Other Myocardial Protection Strategies
While the primary focus here is on modifying the RA procedure, it is also worthwhile to compare this strategy to other myocardial protection techniques used in coronary interventions. Over the years, many different approaches have been touted to minimize myocardial injury:
- Pharmacological Agents: Drugs such as adenosine and other vasodilators have been explored for their protective benefits, though their effects can be variable.
- Remote Ischemic Conditioning: This technique involves inducing brief periods of ischemia in a limb to trigger systemic protective effects; however, the method is not without its own set of challenges.
- Temperature Management during Surgery: Mild hypothermia during procedures like coronary artery bypass grafting has shown some promise, aligning with the underlying idea that cooler conditions can protect heart tissue.
In this context, the low-temperature RA-flush solution represents a hybrid approach, combining a mechanical intervention with a simple yet effective environmental modification. It is a super important reminder that even small adjustments in procedure can yield benefits, especially when dealing with the fine points of myocardial injury and tissue protection.
Patient Perspectives and the Future of Interventional Cardiology
From a patient’s viewpoint, the goal is always to reduce complications and ensure a smoother recovery. When considering complex procedures like RA, where there are many twists and turns, any advancement that can alleviate side effects or reduce the likelihood of myocardial injury is seen as a welcome innovation. Future patient care models may increasingly incorporate such detailed modifications, leading to interventions that are not only more effective but also gentler on the heart.
Addressing Patient Concerns with Clear Communication
It is essential that healthcare providers discuss the rationale behind any new technique with their patients. This includes explaining how a low-temperature flush solution works and why it might reduce the nerve-racking complications typically associated with the RA procedure. Here are some tips for clear communication:
- Simplify the Science: Use everyday language to describe the cooling effect and its benefits on heart tissue.
- Outline the Benefits and Risks: Clearly communicate that while the modification shows promise in reducing some complications, long-term benefits are still under investigation.
- Encourage Questions: Allow patients to ask questions about the process, helping them feel involved and reassured.
Long-Term Vision: Integrating Innovations in Cardiac Interventions
The journey of refining interventional cardiology techniques is ongoing. The innovation of using a low-temperature RA-flush solution is a prime example of how even a minor change can yield multiple benefits during a delicate procedure. Although this study primarily emphasizes the immediate advantages of reduced myocardial injury, it also opens the door for a broader conversation about optimizing procedural safety and efficacy.
Steps Toward Broader Adoption
The gradual transition from academic research to bedside practice involves several phases. The current study is an important step, but further research, peer feedback, and clinical trials with larger sample sizes will be critical in cementing the procedure’s standing. Some strategic actions that could help broaden adoption include:
- Collaborative Research Efforts: Multicenter trials that include a diverse patient population can help validate the early findings.
- Standardizing Protocols: Clear guidelines on when and how to implement low-temperature flush solutions will help smooth the transition from theory to practice.
- Training Programs: Educating interventional cardiologists and cath lab staff on the nuances of this new approach will further ensure its safe application.
The Role of Technology and Data in Enhancing Techniques
Beyond the manual aspects, the future of RA procedures might well lie in integrating advanced data analytics and imaging techniques. For instance, real-time temperature monitoring along with high-definition imaging of the coronary anatomy could allow clinicians to figure a path through the tricky parts of lesion modification. A combination of robotics, artificial intelligence, and advanced sensor technology might soon enable more precise control over procedural conditions—and a more tailored approach to each patient’s unique coronary structure.
Conclusion: A Small Change with Potentially Big Impacts
In sum, the transition to a low-temperature RA-flush solution in interventional cardiology is an innovative step toward reducing myocardial injury during rotational atherectomy. While there are still a few tangled issues and subtle details that need to be carefully examined, early evidence points to significant benefits such as lower incidences of biomarker elevation and fewer transient flow complications.
This opinion editorial emphasizes that, in an area as full of problems as interventional cardiology, even small interventions can lead to meaningful improvements in patient safety. Healthcare providers, device manufacturers, and researchers are all encouraged to take a closer look at these findings and consider how such modifications can be integrated into routine practice.
Ultimately, the goal is to provide treatments that are both effective and gentle on patients—an essential balance when dealing with a procedure carrying as many nerve-racking twists and turns as RA. As further studies confirm or refine these early findings, the adoption of low-temperature RA-flush solutions could soon become a must-have strategy in the armamentarium against calcified coronary lesions.
Key Takeaways
Consider this summary of the main points discussed:
- The low-temperature RA-flush solution shows promise in significantly reducing procedural myocardial injury compared to the room-temperature method.
- Improved local cooling may contribute to fewer instances of transient slow flow, coronary spasms, and reduced inflammatory responses.
- Despite immediate benefits, further research is needed to determine long-term outcomes and to address complex issues like patient selection and procedural variability.
- Operational challenges such as maintaining consistent solution temperatures and revising lab protocols are important factors before wide-scale clinical adoption.
- Advancements in imaging and real-time monitoring could complement these practices, further refining interventional cardiology techniques.
Final Thoughts
The study discussed here represents an exciting step forward in the realm of heart interventions. By rethinking traditional approaches and focusing on controllable factors like temperature, the medical community is gradually uncovering ways to provide safer and more efficient care. As our understanding deepens and as further research is undertaken, innovations such as low-temperature RA-flush solutions are poised to play a key role in the future of patient-centric cardiovascular therapy.
While the road ahead is still a bit tangled with issues that require more detailed exploration, the potential benefits are too significant to ignore. It will be interesting to see how these findings are integrated into clinical practice and whether they will lead to lasting improvements in the success rates of RA procedures. For now, the idea of cooling things down in the cath lab is quickly gaining traction—a small change that might just have a big impact on patient outcomes.
Originally Post From https://www.nature.com/articles/s41598-025-02799-x
Read more about this topic at
Does a Cool Down Prevent Injury?
Cooling interventions for athletes: An overview …

