Revolutionizing Essential Tremor Treatment with No-Touch Brain Surgery
Essential tremor is a movement disorder that has long presented patients and physicians with a number of tricky parts. Historically, those suffering from tremors have battled not only the physical challenges but also the tangled issues of social stigma and professional setbacks. Today, however, modern innovations such as no-touch brain surgery via focused ultrasound are transforming lives in a way that inspires optimism and redefines what is possible in non-invasive neurosurgery.
In this opinion editorial, we take a closer look at the emergence of focused ultrasound as a cutting-edge treatment for essential tremor. We will explore the fine points of the procedure, share a personal journey, and discuss the broader implications that these technological breakthroughs carry for the future of neurological care.
Understanding Essential Tremor and Its Impact
Essential tremor is a common neurological disorder characterized primarily by rhythmic shaking, which often begins in the dominant hand and can progress to affect other areas such as the legs, head, and voice. For many patients, everyday tasks like writing or holding objects become increasingly difficult as the condition advances. The onset is usually subtle, but the small distinctions in the progression of symptoms can have a profound impact on quality of life.
Patients not only battle the physical manifestations but also face the nerve-racking challenges of social misunderstandings. For example, a slight tremor during an important business meeting could be mistakenly interpreted as a sign of nervousness or dishonesty rather than a medical condition. Such experiences underline the importance of effective treatment options that address both the fine details of the condition and the emotional toll it takes.
Personal Journey: Mike’s Experience With Tremor
Mike Mattozzi’s story is both inspiring and poignant. As a teenager in New Hampshire, he first noticed a mild shaking in his dominant hand—a sign that would eventually disrupt the rhythm of his daily life. Over time, the tremor expanded to his other hand, compromising his abilities to perform even the simple acts of holding a pen or using a knife to cut steak.
Mike’s narrative reflects the overwhelming challenges faced by many with essential tremor. When his tremors interfered with his job as a software salesperson, he began to worry about how his colleagues and clients interpreted his condition. “I’d sit down on a sales call, and my hands would be shaking,” he recalled. “What’s the other person thinking? That I’m nervous because I’m lying or hiding something from them.”
Eventually, at age 37, Mike was officially diagnosed with essential tremor. His condition progressively worsened, leading him to reconsider traditional medication-based treatments as they became less effective and, at times, introduced off-putting side effects. Fortunately, advancements in neurosurgery presented an alternative that seemed tailor-made for his situation.
Focused Ultrasound: A Non-Invasive Alternative
Faced with the confusing bits of traditional medication regimens and the risk of invasive brain surgeries, Mike’s care team began exploring alternatives. One promising solution that emerged was focused ultrasound, a procedure that has been refined since its early pivotal research days at Brigham and Women’s Hospital in the 1980s.
This innovative treatment offers a no-touch approach—meaning there is no incision or implanted device needed. Instead, the patient’s head is shaved, a supportive frame is attached to prevent movement, and a series of highly focused sound waves are delivered within an MRI machine to a precise area of the brain. These sound waves generate heat that destroys the tissue responsible for the tremor.
Dr. G. Rees Cosgrove, a neurosurgeon with extensive expertise in functional neurosurgery at Mass General Brigham, explains that this procedure not only sidesteps many of the intimidating aspects of traditional brain surgery but also avoids the nerve-racking complications related to implanted devices. “I call it ‘no-touch brain surgery,’” he says, emphasizing that the process is performed on an outpatient basis. In short, patients can have the procedure and return home after a brief recovery period.
Comparing Focused Ultrasound and Deep Brain Stimulation
The choice between focused ultrasound and deep brain stimulation (DBS) often involves evaluating several key factors. Here is a breakdown that highlights the small distinctions between the two approaches:
| Treatment Aspect | Focused Ultrasound | Deep Brain Stimulation (DBS) |
|---|---|---|
| Invasiveness | Non-invasive; no incisions or implanted devices | Invasive; requires surgical implantation |
| Procedure Complexity | Typically involves a few brief treatment cycles, with minimal recovery time | More complex surgery with longer recovery and potential hardware complications |
| Patient Suitability | Ideal for patients wary of deep surgeries or those with other risk factors tied to surgery | Best suited for patients who can manage implanted technology and require adjustable stimulation |
| Side Effects | Generally limited, with some patients reporting minor headaches | Risk of device-related complications and infection |
This comparative table demonstrates that each treatment has its own set of benefits and tricky parts. The expertise of the neurosurgeon in weighing these factors is essential to achieving the best outcome for the patient.
No-Touch Brain Surgery: The Details and the Process
The science behind focused ultrasound is both fascinating and inherently complex in its fine details. The procedure requires the patient to have his or her head shaved and secured within a special frame that minimizes any head movement. Once positioned in an MRI scanner, hundreds of focused sound waves are targeted at the problematic area in the brain responsible for the tremors.
The treatment is divided into several cycles, typically two to four, each lasting between 15 and 20 seconds. During these cycles, the sound waves produce heat that selectively destroys the malfunctioning tissue causing the tremor. The real-time imaging provided by MRI ensures that each pulse of energy is delivered with pinpoint accuracy. Surgeons are able to monitor the effects immediately and adjust treatment parameters as needed.
According to Dr. Cosgrove, “The key to a successful procedure is understanding the subtle parts of the brain’s response in real time. Our experience has shown that combining deep knowledge of functional neurosurgery with technological advances helps us achieve outcomes that lead to lasting tremor reduction.”
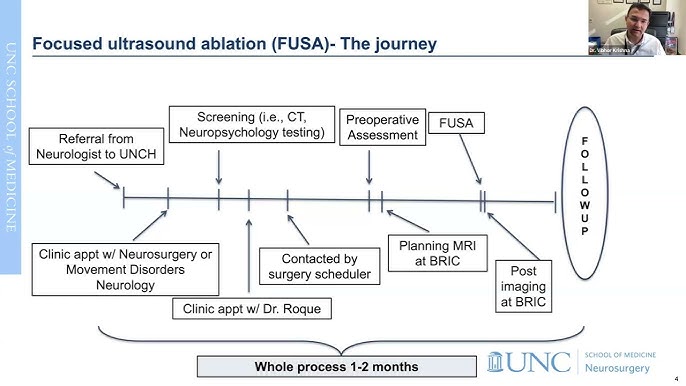
Step-by-Step Overview of the Procedure
For those curious about how the process unfolds, the procedure can be broken down into manageable parts:
- Preparation: The patient’s head is shaved and fitted with a frame to minimize movement during the process.
- Imaging: The patient is placed in an MRI machine, and high-resolution imaging helps identify the exact target area in the brain.
- Treatment Cycles: The procedure consists of multiple cycles, each delivering focused ultrasound pulses with real-time adjustments made by the surgeon.
- Post-Treatment Evaluation: After the cycles are complete, the patient is monitored briefly to evaluate the immediate impact of the treatment.
- Follow-Up: Regular follow-up appointments by phone, video, or in person ensure the long-term success of the treatment.
The Shift to Non-Invasive Neurosurgery
The transition from traditional invasive procedures to high-tech solutions like focused ultrasound represents a significant shift in treating neurological conditions. This shift is not just about technology breakthroughs—it’s also about prioritizing patient comfort, reducing the intimidating risks associated with surgery, and achieving effective, lasting results.
Historically, neurosurgeons had to address both the physical challenges of tremor and the off-putting worry of causing additional complications through invasive surgical methods. Patients who opted for deep brain stimulation had to contend with the reality of having an implanted device that required regular maintenance. In contrast, many find the idea of no-touch brain surgery more appealing due to its simplicity and the fact that it does away with the nerve-racking aspects of traditional brain surgery.
Working through these complicated pieces has led to the development of a procedure that many experts consider to be super important in the landscape of modern neurosurgery. As we continue to get into the subtle parts of the brain, the emphasis is on making treatments more patient-friendly while still being highly effective.
Expert Perspectives on Focused Ultrasound
Neurosurgeon Dr. Cosgrove, who has built a reputation as one of the busiest practitioners in the United States, firmly believes that the best results are achieved when the neurosurgeon is well-versed in both the fine points of focused ultrasound and deep brain stimulation. “You have to be an expert in both to figure a path that is best suited for each individual patient,” he explains.
Assistant Professor Nathan McDonnald from Harvard Medical School, who played a critical role in advancing the technology three decades ago, also stresses that this approach is about more than just treating tremors. It is about restoring confidence to individuals whose lives were once dominated by the tangled issues of uncontrolled shaking. Their collective expertise ensures that each treatment is tailored to the patient’s unique needs, harnessing technology while being mindful of the almost overwhelming challenges posed by essential tremor.
Both experts acknowledge that while every procedure carries its own set of slight differences and hidden complexities, the overarching goal remains the same—providing a safe, effective, and non-invasive option that dramatically improves quality of life.
Key Considerations for Patients and Physicians
When it comes to selecting a treatment plan, there are several critical considerations:
- Patient Preference: Many patients prefer not having invasive devices implanted in their brain. Focused ultrasound offers an appealing alternative.
- Risk Assessment: Physicians must dig into the patient’s overall health, the progression of the disease, and the individual’s ability to handle surgery.
- Treatment Goals: Whether the aim is to alleviate symptoms quickly or to achieve sustained long-term results, treatment objectives play a key role in decision making.
- Long-Term Monitoring: The importance of follow-up visits cannot be overstated. Continuous evaluation helps refine the treatment process and better target future interventions if needed.
Real-World Outcomes and Life-Changing Transformations
Mike’s experience is a testament to the transformative potential of focused ultrasound. On the day of his procedure, the process began rather humbly. Before entering the MRI scanner, he was given simple tasks like drawing lines and circles with a pen, which, on that fateful day, resulted in messy, unpredictable lines. However, after undergoing several treatment cycles, his drawing test transformed dramatically—with perfect circles and straight lines replacing what once were signs of chaos. This visual evidence of his improvement underscored just how powerful the procedure was.
Following the completion of his treatment cycles, Mike underwent a quick evaluation that confirmed the disappearance of his tremors. The rapid turnaround was nothing short of astonishing. In his own words, “It was amazing—that’s the only way I can describe it. An hour after the procedure, I was already waiting for my daughter to pick me up.”
This immediate and dramatic improvement has a profound impact on everyday activities. Tasks that once posed overwhelming challenges suddenly become manageable, allowing patients to regain a sense of independence and confidence. After his initial success with the focused ultrasound treatment on his right hand, Mike later opted to have the procedure performed on his left hand when its condition worsened. Each time, the results were unequivocally positive, ultimately leading to a tremor-free life that has spanned years.
Long-Term Benefits: Consistency and Reproducibility
Long-term data on focused ultrasound is encouraging. Studies have shown that many patients experience a significant reduction—up to 73%—in their tremor symptoms for at least five years post-treatment. Moreover, the procedure’s reproducibility is a crucial advantage. In the rare cases where tremors significantly return, the procedure can be repeated with similar levels of success.
The consistency of these outcomes strongly suggests that focused ultrasound is not merely a temporary fix but a sustainable solution for managing essential tremor. With only an estimated 6% of patients needing a redo, as noted by Dr. Cosgrove from among the 700 cases he has performed, the statistics speak clearly to the reliability and effectiveness of this innovative treatment.
Future Directions in Non-Invasive Brain Surgery
While the current success of focused ultrasound is undeniably transformative, the journey does not stop here. The field of neurosurgery continues to evolve rapidly, and many are eager to see how further research and technological advancements could expand the applications of non-invasive treatments. The promising results in managing essential tremor open the door for applying similar techniques to other neurological conditions.
Ongoing research is taking a closer look at how focused ultrasound might be used to target conditions such as Parkinson’s disease, chronic pain, and even certain psychiatric disorders. Experts believe that as our understanding of the brain matures, the subtle parts of these disorders can be treated with ever-greater precision. The hope is that one day, a range of conditions loaded with issues and challenging twists could be managed without the need for invasive surgery.
Emerging Technologies and Combined Approaches
One exciting prospect is the integration of focused ultrasound with other treatment methods. Combining its non-invasive profile with advances in imaging technology and telemedicine could further enhance patient outcomes. For instance, real-time data analytics and AI-powered imaging improvements might allow for even more refined targeting of the affected brain tissue.
As technology progresses, we might see personalized treatment plans that are tailored not only to the specific condition but also to the individual’s unique brain anatomy. This level of customization would represent a major step forward in determining how to best manage the tangled issues of neurological disorders.
Considering the current benefits and the possibility of combining different technological approaches, the future of non-invasive brain surgery appears bright. It stands as a beacon for what is achievable when we work through the challenging bits of medical research with innovation and compassion.
Patient Empowerment and the Role of Follow-Up Care
Beyond the immediate surgical success, long-term follow-up care is essential for sustaining the benefits of focused ultrasound. At Brigham and Women’s Hospital, patients like Mike undergo several check-ups—via phone, video, or in-person visits—at intervals of one week, one month, and three months post-procedure, and then annually thereafter. These ongoing consultations allow physicians to adjust any factors that might lead to a recurrence of symptoms and to fine-tune their approach based on the patient’s progress.
This systematic follow-up is not merely a precaution but an indispensable part of contemporary medical care. It represents a commitment to patient empowerment, ensuring that every individual receives the supervision necessary to maintain their improved quality of life. In many cases, the success of focused ultrasound is not just measured by the absence of tremors immediately after the procedure but by the sustained improvement over many years.
Follow-up care also plays a key role by providing patients with reassurance. Through these regular interactions, they can dig into any subtle details or new issues that might arise, ensuring their treatment remains effective. This attentive approach to care embodies the modern spirit of personalized medicine, where treatments are continuously refined based on real-world outcomes and patient feedback.
How Continuous Monitoring Improves Outcomes
Continuous monitoring after focused ultrasound brings several benefits:
- Early Detection of Recurrences: Regular check-ups help in identifying even slight differences in symptom progression, allowing for prompt intervention if tremors begin to reappear.
- Data-Driven Adjustments: Feedback from follow-up visits enables physicians to tweak targeting parameters, ensuring the treatment remains as effective as possible.
- Patient Reassurance and Confidence: Consistent monitoring fosters a sense of security in patients, helping them manage any anxiety related to the persistence or return of symptoms.
- Long-Term Research Benefits: The data collected from ongoing follow-up visits contributes to research, which may pave the way for even better treatments in the future.
Societal Implications of Non-Invasive Neurosurgery
Beyond the realm of individual patient care, the rise of focused ultrasound has broader societal implications. The ability to treat essential tremor without resorting to invasive procedures can lead to reduced healthcare costs, lower risks of surgical complications, and an overall improvement in patient welfare. As more healthcare providers gain confidence in these methods, millions of patients could potentially avoid the intimidating risks associated with traditional brain surgeries.
The development of this technology also reflects a broader trend towards less invasive treatment solutions in modern medicine. As society continues to grapple with the ever-evolving challenges of chronic diseases, the preference for treatments that minimize risk, reduce hospital stays, and promote quick recovery becomes increasingly essential.
On a larger scale, the success of non-invasive neurosurgery could shift the focus of healthcare systems from reactive interventions to proactive, patient-centered approaches. Investing in research and widening the availability of advanced treatments like focused ultrasound may eventually relieve some of the societal burdens associated with long-term neurological care.
The Economic and Healthcare Benefits
When we consider the economic impact, several key points emerge:
- Reduced Hospital Stays: Patients undergoing no-touch brain surgery can often return home the same day, reducing inpatient costs.
- Lower Risk of Complications: Non-invasive procedures generally diminish the need for follow-up surgeries and reduce the risk of infection or device-related issues.
- Enhanced Workforce Productivity: Patients who overcome debilitating tremors are better able to return to their normal activities, improving overall workforce productivity.
- Streamlined Healthcare Resources: Fewer complications and shorter recovery times mean that healthcare providers can allocate resources more efficiently, ultimately benefiting the broader community.
Looking Ahead: Future Challenges and Opportunities
While the current advancements in no-touch brain surgery are promising, there are still some tricky parts and complicated pieces that researchers and clinicians must carefully address. For one, the technology demands a very high level of precision, making the expertise of the neurosurgeon absolutely super important. The subtle details of how brain tissue reacts to ultrasound waves are still being actively studied, and there is always room for improvement in refining the targeting techniques.
Another area full of problems is the broader accessibility of these advanced treatments. While centers of excellence like Mass General Brigham and Brigham and Women’s Hospital are leading the way, ensuring that patients everywhere have access to non-invasive solutions remains a critical challenge. This involves not only training more specialists in focused ultrasound but also updating hospital facilities and investing in high-end imaging technologies.
Furthermore, as research digs into other potential applications of focused ultrasound, the process will inevitably reveal additional twists and turns. Whether it’s managing Parkinson’s disease or addressing certain psychiatric conditions, the possibility of expanding this technique’s use is both exciting and slightly tense—given the inherent uncertainties of pioneering medical treatments.
Bridging the Gap Between Innovation and Accessibility
Addressing these challenges requires a concerted effort on several fronts:
- Investment in Research: Continued funding and robust clinical trials are essential to further our understanding of focused ultrasound and similar technologies.
- Expanding Training Programs: Encouraging neurosurgeons to get into both functional neurosurgery and the latest imaging techniques can help standardize and spread these treatments.
- Policy Initiatives: Healthcare policymakers need to consider how to make advanced, non-invasive procedures more accessible, especially in regions that currently lack high-resolution MRI technology.
- Collaborative Efforts: Continued collaboration between research institutions, hospitals, and technology developers will be critical in overcoming the tangled issues of scaling these innovations.
Conclusion: A Paradigm Shift in Neurological Care
Focused ultrasound represents an exciting leap forward in the management of essential tremor—a condition that has traditionally weighed heavily on patients’ daily lives. By eliminating the need for incisions or implanted devices, this procedure breaks away from the nerve-racking complications and surgical risks historically associated with brain surgery. The story of Mike Mattozzi is a compelling example of how such advances are not only medically transformative but also life-changing from a human perspective.
As we dive in to the future of non-invasive neurosurgery, the benefits for both individual patients and society at large are undeniable. With continued research, expanding access, and an unwavering commitment to patient-centered care, the medical community is positioned to field new treatments that tackle the hidden complexities of neurological disorders.
In this new era of neurological care, the goal is clear: to provide safe, effective, and sustainable treatment options that empower patients to regain control of their lives. Whether you are a patient facing the overwhelming challenges of essential tremor or a healthcare provider searching for innovative solutions, the advancements in focused ultrasound offer a beacon of hope—a promise backed by growing expertise, scientific breakthroughs, and a commitment to excellence that is reshaping modern medicine.
For those who have followed the journey of this no-touch brain surgery, it becomes evident that the future is not solely about fixing a problem—it’s about restoring dignity, confidence, and the ability to live life unencumbered by the intimidating hurdles of a chronic condition. As we continue to figure a path through the ever-changing landscape of modern neurosurgery, one thing remains certain: the evolution of essential tremor treatment is paving the way for a broader transformation in how we approach and manage neurological disorders as a whole.
Ultimately, the success of focused ultrasound challenges us to rethink our approach to complex neurological conditions and to adopt a model of care that is as patient-friendly as it is clinically effective. With every new study and every patient story like Mike’s, the evidence accumulates in support of a future where the fine points of brain treatment are managed with precision, minimal risk, and maximum benefit for those in need.
This paradigm shift is a testament to what can be achieved when innovation meets compassion—a reminder that even the most intimidating medical challenges can be overcome with the right blend of technology, expertise, and human determination.
Originally Post From https://www.massgeneralbrigham.org/en/about/newsroom/patient-stories/mikes-essential-tremor
Read more about this topic at
Mike’s Essential Tremor Patient Story
New treatment for tremors: Cutting-edge brain surgery with …