Exploring the Biomechanical Landscape of Femoropopliteal Arteries
The recent study analyzing the biomechanical differences in femoropopliteal arteries between healthy individuals and patients who have undergone revascularization procedures offers a unique window into the subtle yet significant changes in arterial mechanics. This editorial takes a closer look at the study’s implications, examining the fine points behind the mechanical properties of these essential blood vessels and their broader impact on cardiovascular health.
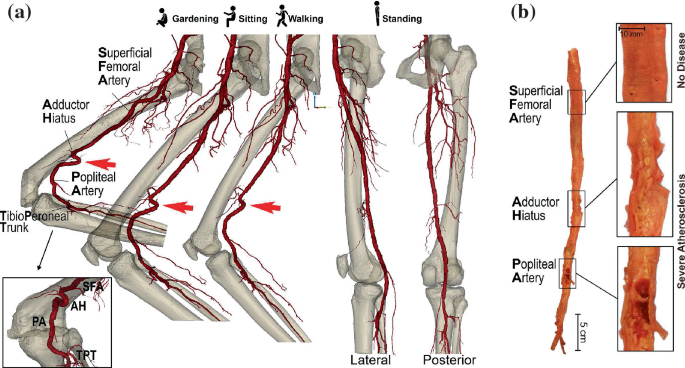
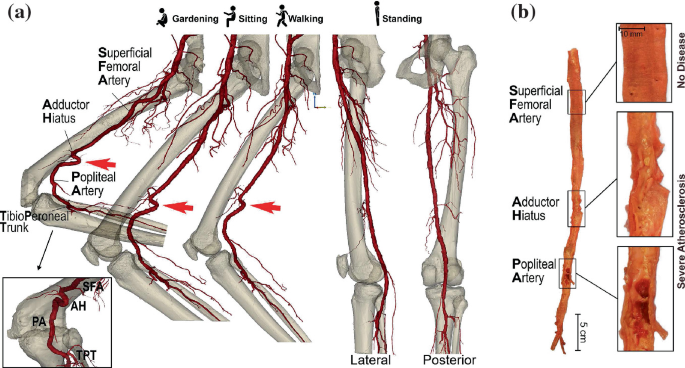
Femoropopliteal arteries, which play a critical role in supplying oxygenated blood to the lower limbs, are subject to countless twists and turns throughout life. As individuals age or develop vascular issues, these vessels may become altered in structure and function. The study led by researchers Gostev, Osipova, and Volkova digs deep into comparing the mechanical behavior of these arteries in healthy individuals versus those who have received revascularization procedures.
In this opinion piece, we will dig into the research findings while discussing the tricky parts of arterial biomechanics, the impact of medical interventions on vascular function, and the potential future benefits for patients dealing with lower limb circulatory challenges.
Understanding the Study Methodology and Its Practical Implications
This research was designed to take a closer look at the mechanical properties of femoropopliteal arteries under normal, physiological conditions compared to those in a revascularization context. The team assessed various parameters of arterial behavior that could influence the success of interventions and long-term vascular health. By comparing the vessels from healthy individuals with those from patients who had undergone revascularization, the study provides insight into how different factors alter the arteries at a fundamental level.
Key Research Focus Areas
The study focused on several critical components to get a balanced view of vascular performance. Among these were:
- Arterial compliance: How flexible or stiff the artery becomes.
- Wall mechanics: The response of the arterial wall under various pressure conditions.
- Flow dynamics: The ease with which blood flows through the vessel.
- Structural integrity: The physical robustness of the vessel following intervention.
Each of these points involves subtle details that matter greatly when assessing how revascularization affects overall blood flow and artery stability. Patients often face overwhelming and nerve-racking challenges when trying to understand the consequences of such invasive procedures. By getting into the nitty-gritty of arterial behavior, researchers are offering a clearer picture of both the benefits and the potential limitations of modern medical interventions for vascular diseases.
Data Comparison: Healthy Versus Post-Revascularization Arteries
A simplified comparison of the two groups can be illustrated using the table below. This table provides a concise summary of how key parameters differ between healthy arteries and those that have undergone revascularization.
| Parameter | Healthy Individuals | Revascularization Patients |
|---|---|---|
| Arterial Compliance | Optimal flexibility | Increased stiffness in certain segments |
| Wall Mechanics | Responsive to natural pressure changes | Altered response due to scarring or artificial supports |
| Flow Dynamics | Smooth, unobstructed flow | Variable flow patterns with possible turbulence |
| Overall Structural Integrity | Maintains original structural composition | May have repaired sections with different elasticity |
This table encapsulates the little twists and challenging details that clinicians must consider when planning treatment. Each parameter carries a load of subtle details that can have a tremendous impact on a patient’s recovery and quality of life after revascularization.
Decoding the Tricky Parts of Arterial Biomechanics
Diving in to understand vascular mechanics requires one to figure a path through several complicated pieces that may be overwhelming at first glance. Many of the arterial changes that occur after revascularization are not merely superficial—they reach into the small distinctions of tissue behavior, the interplay between the biological response and mechanical forces, and the way in which blood flow patterns become rerouted.
Understanding Arterial Compliance and Its Importance
Arterial compliance, often characterized by the ability of a vessel to expand and contract with blood pressure variations, is a super important aspect of cardiovascular health. In healthy arteries, compliance maintains a harmonious balance between elasticity and stability. However, after medical interventions such as revascularization, this flexibility may decrease. This decrease can be attributed to factors such as:
- Tissue scarring and remodeling
- The presence of stents or other mechanical fixtures
- Changes in the vessel’s natural biochemical environment
When vessels become less compliant, the twists and turns introduced can lead to inefficient blood flow. This may increase the stress on the heart, potentially setting the stage for further complications over time. Patients and clinicians alike must consider these subtle parts of vascular mechanics, weighing the benefits of restored flow against the long-term ramifications of a stiffer artery.
The Impact of Wall Mechanics on Vascular Health
The mechanical behavior of the arterial wall is another critical factor in managing limb circulation. For healthy arteries, the ability to adjust to internal pressures is a key element in maintaining good vascular health. However, following revascularization, this ability may become compromised due to changes in the wall’s structure.
Key issues include:
- Stiffening of the arterial wall: Reduced ability to absorb shocks from blood pressure variations.
- Alteration in collagen and elastin composition: These natural proteins, which help the artery to stretch and then recoil, can be affected by post-procedural healing processes.
- Stress distribution: Areas of localized stress can develop where repairs were made, making these segments more vulnerable to future injury.
These problematic factors combine to create a situation that is full of problems—a scenario that physicians have to steer through and manage on a day-to-day basis. In some ways, the differences in wall mechanics represent the hidden complexities in what might seem like a straightforward medical intervention.
Evaluating the Benefits and Challenges of Revascularization Procedures
Revascularization has long been a cornerstone treatment for occlusive arterial diseases. However, the study indicates that the mechanical changes following such procedures are characterized by both improvements in blood flow and the introduction of new, unintended challenges. To understand this, it is crucial to work through the following issues:
Improved Blood Flow Versus Mechanical Trade-Offs
On one hand, revascularization is designed to restore unobstructed blood flow. This is often achieved by clearing blockages, inserting stents, or bypassing problematic segments. Patients usually experience dramatic improvements in symptoms such as pain and mobility issues. On the other hand, these interventions bring along tangled issues related to altered biomechanics of the arterial wall.
Some of the trade-offs include:
- Restoration of flow: Immediate benefit in terms of oxygen and nutrient supply to the limb.
- Altered vessel dynamics: A changed response to pulsatile blood pressure that could lead to long-term complications if not closely monitored.
- Risk of re-narrowing (restenosis): Despite the initial success, some patients may experience a gradual re-clogging of the vessel due to neointimal hyperplasia or other factors.
These issues remind us that while revascularization techniques are a super important life-saving tool, understanding the full environment of arterial behavior—even with repairs—requires unpacking the small distinctions that lie beneath the surface. The delicate balance between improved function and potentially problematic mechanical changes underscores the need for careful and ongoing evaluation post-procedure.
Patient Perspectives and Lifestyle Considerations
While the study is steeped in the technical details of arterial biomechanics, it is also vital to consider the everyday life of patients. From the perspective of someone facing this type of intervention, the medical data may seem overwhelming, but it ultimately translates into real-life decisions about health, activity, and long-term treatment strategies.
Key points from a patient perspective include:
- Understanding procedure outcomes: Patients want to know that the improvement in blood flow is sustained over time despite any changes in vessel elasticity.
- Adapting to physical limitations: The fine shades of arterial function may dictate how much exercise is safe and how vigorous activity should be.
- Long-term monitoring: Regular follow-up appointments are necessary to track any evolving changes in arterial wall behavior.
This broader view highlights that while scientists and clinicians may be busy poking around the hidden complexities of blood vessel mechanics, the everyday impact on a patient’s quality of life and overall cardiovascular well-being is a matter of key importance. Counseling and education are essential in helping patients to figure a path that balances intervention benefits with potential risks.
Exploring Future Directions in Arterial Health Research
Looking forward, the research into femoropopliteal artery mechanics opens several new avenues for both clinical application and further scientific inquiry. As we get into the details of how these arteries behave and how medical interventions alter their structure, several new challenges and opportunities emerge.
Innovative Technologies and Monitoring Techniques
Current advancements in imaging and diagnostic tools are already making it easier to observe the subtle details of arterial function. The use of ultra-high-resolution scanners, for instance, allows researchers to take a closer look at the delicate balance of arterial tissue before and after intervention. Future directions in this area include:
- Real-time vascular imaging: Techniques that provide live feedback on arterial behavior during interventions.
- Advanced simulation models: Computer models that can predict the mechanical outcomes of different revascularization techniques.
- Wearable monitoring devices: Technologies that enable continuous assessment of blood flow dynamics and arterial stiffness in everyday life.
These innovative tools not only help bridge the gap between research and clinical practice but also empower patients to take an active role in monitoring their cardiovascular health. With improved data collection and analysis methods, it becomes possible to manage the often intimidating and nerve-racking process of long-term vascular care more effectively.
Clinical Implications and Personalized Treatment Strategies
A major takeaway from the study is the need for personalized treatment plans that account for the individual characteristics of each patient’s vascular system. This approach could help overcome some of the off-putting aspects of a one-size-fits-all model. Personalized strategies might include:
- Tailored revascularization plans: Using detailed biomechanical data to choose the best procedural method for each patient.
- Customized follow-up care: Adjusting the frequency and type of monitoring based on the unique arterial behavior observed in each case.
- Risk stratification models: Predictive models that identify patients who may be more likely to experience complications like restenosis or altered vessel compliance.
Personalized medicine in vascular care is an area where understanding the subtle details of arterial mechanics becomes a super important asset. When physicians can get into the nitty-gritty about how a patient’s own vessels react to intervention, they are better equipped to steer through the potential pitfalls and design a treatment strategy that maximizes long-term benefits.
Integrating Research Insights into Everyday Clinical Practice
The fruit of this study is not only academic—it has profound practical implications for everyday clinical care. Many clinicians, when trying to find their way through the tangled issues of arterial revascularization outcomes, can benefit from the insights provided by such detailed investigations.
Bridging the Gap Between Research and Bedside Care
Translating detailed biomechanical research into practical clinical guidelines is a challenging process filled with many twists and turns. Key steps in this translation process include:
- Educating healthcare providers: Physicians, nurses, and vascular technologists need to be briefed on the new findings and how they might affect both procedural choices and post-procedural care.
- Updating treatment protocols: Clinical practice guidelines should integrate the latest research findings, ensuring that patients receive care that reflects current understanding.
- Encouraging interdisciplinary communication: Surgeons, interventional radiologists, and primary care providers must work together, sharing insights and data to optimize patient outcomes.
- Implementing patient-centered care: This involves keeping patients informed about the fine shades of possible risks and benefits, thus empowering them to play an active role in their treatment decisions.
In many ways, the work is far from complete. More research is needed to iron out the confusing bits of how arterial behavior changes over time—a challenge that remains both appealing to researchers and immediately beneficial to patients.
Creating Collaborative Research Networks
Given the layered issues involved in understanding arterial mechanics, collaboration among different research institutions is key. By pooling resources and data, scientists can better figure a path through the tangled issues that emerge in the study of vascular health. Benefits of such collaborative efforts include:
- Data sharing: A broader data pool helps in identifying subtle distinctions that may have been overlooked in smaller studies.
- Standardization of techniques: Collaborative research can lead to standardized protocols that ensure consistency and accuracy in measurements.
- Interdisciplinary approaches: Insights from biomechanics, materials science, and even computational modeling enrich our understanding of vascular changes post-intervention.
- Enhanced patient outcomes: Ultimately, the more doctors understand the detailed parts of arterial behavior, the better they can tailor interventions to individual patient needs.
Such interdisciplinary networks make it possible to sort out the hidden complexities of arterial biomechanics while also focusing on developing improved strategies for revascularization and long-term vascular care.
Addressing the Overwhelming Aspects of Vascular Interventions
Living with a condition that requires revascularization can be an intimidating experience for patients. The uncertainty and the many tangles of both mechanical and biological responses create a situation that is off-putting and often nerve-racking.
Navigating the Patient Experience
For many patients, the decision to undergo revascularization is accompanied by a mix of relief and apprehension. On the one hand, the prospect of improved blood flow and diminished symptoms offers hope; on the other, the fear of potential complications can cast a shadow over the entire process. Patients often face several overlapping concerns such as:
- Understanding the procedure: What exactly will change in the structure of their arteries?
- Long-term effects: How will the decreased arterial compliance or altered wall mechanics affect daily life?
- Follow-up care: What kind of monitoring and additional interventions might be necessary?
These are not merely clinical questions but very personal ones that impact the overall quality of life. By sharing insights gleaned from in-depth research studies, healthcare providers can help demystify the confusing bits and make the process feel less overwhelming. Education and open dialogue are essential in easing the off-putting nature of such treatments.
Empowering Patients Through Information
One of the most super important aspects of modern healthcare is ensuring that patients are well-informed. When individuals are given clear, accessible information about what to expect before, during, and after a revascularization procedure, they can make more confident decisions. Some effective strategies include:
- Simplified visual aids: Tables, charts, and infographics can help break down the complicated pieces of research findings into digestible insights.
- Interactive seminars: Allowing patients to engage with healthcare professionals to discuss their specific case details helps to connect overarching research to personal experiences.
- Written resources: Brochures and online content that use everyday language and relatable metaphors can bridge the gap between technical jargon and patient understanding.
These methods help manage the overlapping issues of both physical and informational challenges that patients face. Ultimately, the goal is to reduce the intimidating aura of complex medical procedures by making the fine details more understandable and accessible.
Future Perspectives: Charting a Course for Improved Vascular Health
As research into the biomechanical behavior of femoropopliteal arteries moves forward, the opportunities to improve patient care and outcomes become even more promising. The integration of sophisticated diagnostic tools, personalized treatment strategies, and enhanced patient education programs heralds a new era in vascular medicine.
Bringing Advanced Diagnostics to the Forefront
One promising future direction is the implementation of advanced diagnostic protocols. These protocols aim to catch even the slight differences in vascular performance that could indicate early signs of complications. Some of these emerging technologies include:
- High-resolution vascular imaging: Techniques that can monitor the minute details of arterial wall changes in real time.
- Biochemical markers: Blood tests designed to pick up on subtle changes in the extracellular matrix of the arterial walls.
- Artificial intelligence (AI) tools: Systems capable of analyzing complex patterns from a range of patient data to predict long-term outcomes.
As these technologies mature, they will provide clinicians with the super important data needed to make informed decisions about both immediate interventions and long-term management strategies.
Personalized Vascular Therapy: A Game Changer
The crossover between detailed biomechanical research and clinical application is perhaps best exemplified by the move towards personalized vascular therapy. The idea is simple: use the subtle details uncovered by research to tailor treatments that are uniquely suited to each patient’s anatomical and physiological profile.
Benefits of personalized therapy include:
- Optimized stent selection and placement: Based on detailed imaging and mechanical data.
- Customized rehabilitation protocols: Rehabilitation plans focusing on gradual restoration of arterial function and improved limb mobility.
- Targeted pharmacotherapy: Using medications that specifically address the altered biochemical environment of post-revascularization arteries.
These strategies are designed to take the guesswork out of treatment, effectively managing your way through the intricate, sometimes confusing bits of post-procedural care and offering patients a clearer, more hopeful path to recovery.
Expanding Clinical Trials and Collaborative Studies
Looking forward, it is crucial to expand the scope of clinical trials that investigate the long-term outcomes of revascularization. Collaborative studies involving multiple research centers will help to sort out the fine shades of differences in arterial mechanics between individuals. Such trials are likely to:
- Provide a larger dataset for refining treatment protocols.
- Identify new risk factors linked to reduced arterial compliance.
- Enhance our understanding of the patient experience across different demographic groups.
The more we understand about these hidden complexities, the better we can design interventions that are both safe and effective. These studies are on the cutting edge of vascular medicine and will likely form the bedrock of future treatment guidelines.
Conclusion: Weighing the Research in the Real World
The study on femoropopliteal arterial biomechanics between healthy individuals and patients post-revascularization provides a detailed look into the ways in which these critical blood vessels change after an intervention. By comparing aspects such as arterial compliance, wall mechanics, and flow dynamics, researchers have identified both promising benefits and challenging trade-offs in current treatment modalities.
For clinicians, patients, and researchers alike, there is a clear message: while revascularization can restore essential blood flow and alleviate immediate symptoms, the long-term management of vascular health requires careful attention to the fine points of arterial behavior. Whether in the form of innovative diagnostics, personalized treatment regimens, or more effective patient education, the future of vascular intervention looks set to build on these important research findings.
In conclusion, the insights from this study help to peel back the layers of confusion surrounding revascularization outcomes. The delicate balance between improved blood flow and altered biomechanical properties underscores the need to consider every small distinction when formulating treatment plans. As research advances and our tools for analysis become ever more precise, we can expect a shift toward more tailored, patient-focused approaches that aim to overcome the intimidating challenges of vascular disease management.
By embracing these advances and working together—clinicians, researchers, and patients alike—we can hope to find our way through the tangled issues of arterial health. Ultimately, understanding these tricky parts is not just a matter of academic interest; it is a step toward better, more effective therapies that improve everyday lives.
Originally Post From https://www.geneonline.com/study-analyzes-biomechanical-differences-in-femoropopliteal-arteries-between-healthy-individuals-and-revascularization-patients/
Read more about this topic at
Comparative Study of Human and Murine Aortic …
Comparative biomechanical and structural evaluation of …